You are here: Urology Textbook > Surgical Management > Foley catheter
Foley Catheter: Indications, Complications, and Insertion Technique
Indications for Transurethral Foley Catheters
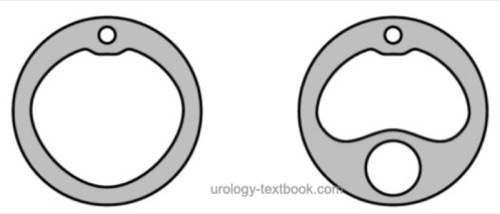
Two-way catheters with a thick channel for urine drainage and a thin channel for balloon occlusion are used for indwelling catheterization [Fig. Catheter cross-sections]. The catheters used differ in shape and material depending on the indication for drainage of the lower urinary tract.
 |
- Intermittent catheterization: For sterile urine collection (alternative to midstream urine or suprapubic puncture), before cystography or urodynamics, residual urine measurement (if sonography is not available), for intravesical therapy (BCG or mitomycin C), for the treatment of urinary retention (intermittent self-catheterization).
- Diagnostic indications: Determination of urine output (after surgery, ICU). Thin catheters (12–16 Fr in adults) are sufficient.
- Therapeutic indications: urinary retention, low-pressure urine drainage after surgery or injuries to the urinary tract, severe urinary tract infections in patients with internal ureteral stents or vesicoureteral reflux, perioperatively during major surgery. In patients with hematuria or injuries to the urinary tract, thicker catheters should be used for safe urine drainage (18–22 Fr in adults).
- Palliative care: for urinary incontinence or immobility in pre-terminal patients, thin catheters (12–16 CH in adults) are sufficient. See also Table comparison of transurethral and suprapubic catheter for the advantages and disadvantages.
- Irrigation catheters: used to prevent bladder tamponade in patients with significant hematuria or after urogenital surgery. Irrigation catheters are large-bore 3-way catheters (20–24 Fr) with one channel for urine drainage, one channel for the irrigation solution, and one thin channel for the balloon occlusion [Fig. Catheter cross-sections]. There is a wide variety of catheter tips in terms of shape and arrangement of the drainage eyes (Nelaton, Tiemann, Couvelair, Dufour, or Mercier, see fig. Catheter tips).
| Transurethral catheter | Suprapubic catheter | |
| Advantages |
|
|
| Disadvantages |
|
|
Contraindications for Transurethral Foley Catheters:
- Suspected posterior urethral injury (insertion with cystoscopy or retrograde urethrography)
- Non-passable urethral stricture or false passage
- Transurethral catheters should be avoided in acute prostatitis or epididymitis
Catheterization: Technique of Transurethral Catheterization in Men
The use of a catheter set and the assistance of a second person facilitate catheter placement.
- Supine position, lower body fully exposed. Place a waterproof drape underneath.
- Prepare equipment, perform hygienic hand disinfection, and put on sterile gloves.
- Grasp the penis proximally to the glans with the left hand and stretch it upward (left hand becomes non-sterile). All further steps are performed with the sterile right hand.
- Disinfect the penis with swabs and forceps.
- Slow injection of sterile lubricant with local anesthetic into the urethra. Cover the genital area with a sterile fenestrated drape.
- Advance the sterile catheter under aseptic conditions. Orient the curvature of the catheter tip at 12 o’clock. When passing the sphincter, lower the penis slightly to straighten the urethra.
- Inflate the catheter balloon with distilled water or a 10% glycerin–water solution.
Difficult situations during transurethral catheterization:
Urethral strictures, false passages from failed attempts, or prostatic disease may complicate or even prevent transurethral catheterization. If a suprapubic catheter is not an option, the following measures may be considered:
- For urethral strictures: stepwise dilation with single-use catheters or urethral sounds. Caution: risk of false passage. A safer approach is placement of a guidewire followed by dilation with ureteral dilators, Amplatz dilators, or with the aid of an access sheath for flexible ureteroscopy.
- For false passage: placement of a (hydrophilic) guidewire using a cystoscope, or blindly with fluoroscopic or sonographic control. Catheter placement over the guidewire (open-tip catheter).
Technique of Transurethral Catheterization in Women:
- Supine position, lower body fully exposed, legs flexed and abducted.
- Place a waterproof drape underneath. Prepare equipment, perform hygienic hand disinfection, and put on sterile gloves.
- Use the left hand to separate the labia (left hand becomes non-sterile). All further steps are performed with the sterile right hand.
- Disinfect the vulva with swabs and forceps, then cover the genital area with a sterile fenestrated drape.
- Lubricate the catheter and advance it through the urethral meatus under aseptic conditions.
- Inflate the catheter balloon with distilled water or a 10% glycerin–water solution.
Difficult situations:
Obesity or vulvar atrophy may obscure the external urethral meatus. The following techniques may facilitate catheterization:
- Blind catheter insertion guided by a palpating vaginal finger
- Catheterization in lithotomy position, if necessary, with a speculum
- For urethral strictures: see above
Complications of Transurethral Catheterization:
Injuries:
Particularly with rigid catheters, urethral injury, perforation, or false passage may occur due to a mucosal fold or urethral narrowing.
Urethral strictures:
Strictures may develop from infection or ischemic urethral injury. Risk factors include duration of catheterization, catheter size, and traction on the catheter.
Biofilm formation and obstruction:
The catheter surface is covered within hours by a host-derived biofilm of proteins and macromolecules. Bacterial colonization thickens the biofilm, which may obstruct the lumen if displaced or excessive in thickness.
Ascending infection:
Despite closed drainage, bacteria ascend extraluminally along the biofilm into the bladder. The bacteriuria rate increases by 3–10% per day of catheterization, with risk of clinical infection (cystitis, urethritis, prostatitis, epididymitis, or pyelonephritis). See also section urinary tract infections.
Balloon deflation failure:
Salt precipitation, damage to the balloon channel or valve may prevent balloon deflation and catheter removal. First, cut the catheter 10 cm proximal to the meatus to correct a valve defect. If unsuccessful, perforate the balloon channel with a rigid, fine stylet (e.g., from a ureteral catheter). If this fails, perform an ultrasound-guided suprapubic puncture of the balloon with a filled bladder.
Other complications:
Bladder stones; squamous cell bladder carcinoma (with very long-term catheterization).
| Bladder catheter | Index | Suprapubic catheter |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Gambrill B, Pertusati F, Hughes SF, Shergill I, Prokopovich P. Materials-based incidence of urinary catheter associated urinary tract infections and the causative micro-organisms: systematic review and meta-analysis. BMC Urol. 2024 Aug 30;24(1):186. doi: 10.1186/s12894-024-01565-x.
Robinson J. Urethral catheter selection. Nurs Stand. 2001 Mar 7-13;15(25):39-42. doi: 10.7748/ns2001.03.15.25.39.c2993.
Sökeland, J., Brühl, P., Hertle, L., and Piechota, H. (2000).
Katheterdrainage der Harnblase heute.
Dtsch Arztebl, 97(4):A167-A174.
 Deutsche Version: Indikationen und Legetechnik für transurethrale Dauerkatheter
Deutsche Version: Indikationen und Legetechnik für transurethrale Dauerkatheter
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.