You are here: Urology Textbook > Surgical Management > Suprapubic catheter
Suprapubic Catheter: Indications, Complications, and Insertion Technique
Indications for Suprapubic Catheters
 |
The suprapubic catheter [Fig. placement of a suprapubic catheter] is considered a better alternative to the transurethral Foley catheter in selected situations. See the table transurethral vs. suprapubic catheter for the advantages and disadvantages of both approaches.
| Transurethral catheter | Suprapubic catheter | |
| Advantages |
|
|
| Disadvantages |
|
|
Long-term catheterization:
The method of choice for long-term catheterization (lasting over a week), especially in men.
Voiding trials:
A suprapubic catheter allows easy assessment of post-void residual urine.
Contraindications for transurethral catheters:
Urethral strictures, false passage, and initial management of urethral injury when transurethral catheterization is not feasible.
Infections:
In cases of acute prostatitis or epididymitis with impaired bladder emptying.
Contraindications for a Suprapubic Catheter
Absolute contraindications:
Bladder cancer, lower abdominal tumors displacing the bladder, coagulopathy, relevant skin diseases at the catheter entry site, and cross-over bypass.
Relative contraindications:
Insufficiently filled bladder (<200 ml), previous lower abdominal surgery, ileus, pregnancy, morbid obesity.
Catheter materials for suprapubic catheterization
For short-term use (perioperative indication), one-way catheters made of polyurethane or PVC are often employed and secured to the skin with a suture. For long-term use, a silicone indwelling catheter with balloon fixation should be used. The catheter balloon eliminates the need for skin sutures and reduces the risk of infections at the catheter entry site. Suprapubic catheters feature a short Nelaton tip and a small balloon volume, designed to enhance patient comfort.
Technique of Percutaneous Suprapubic Catheterization
Use of a catheter set and the assistance of a second person to facilitate the catheter placement. Consider an open approach with a mini-cystostomy in difficult situations (see relative contraindications above).
- Supine position with slight Trendelenburg tilt. Shave the puncture site. Fill bladder with at least 200 ml saline (via intermittent catheter) and perform ultrasound of the catheter entry site (check for bowel interposition or bladder pathology).
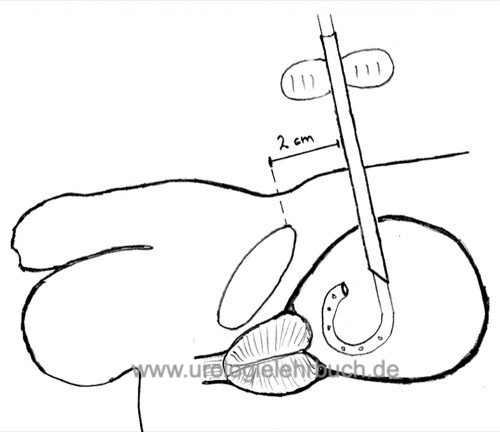
- Proceed with sterile gloves. Disinfect and drape the lower abdomen. The catheter entry site is midline, 1–2 fingerbreadths above the symphysis. Apply local anesthesia: 10–20 ml lidocaine for the catheter entry site, above and below the rectus fascia. Perform a test puncture with aspiration using the local anesthesia syringe; memorize the syringe angle and depth (especially important in obese patients).
- Prepare the hollow trocar (10–12 Ch) with an appropriate catheter. Make a small vertical skin incision with a scalpel. Advance the trocar into the bladder until urine appears, then advance the catheter and inflate the balloon. Withdraw and remove the trocar.
- Pull back the suprapubic catheter to the marker or until the balloon reaches the bladder wall. If necessary, secure the (one-way) catheter with a suture. Apply a dry dressing and secure the catheter against traction.
Complications of Suprapubic Puncture:
Perivesical or intravesical bleeding, malpuncture with possible injury to adjacent organs (bowel) or large vessels (beware of a cross-over bypass). Infection or abscess formation at the catheter entry site or catheter tract (Ahluwalia et al., 2006).
Side effects and complications of suprapubic catheterization:
Catheter dislodgement (balloon leak or rupture), biofilm formation with encrustation and infection, bladder stones, squamous cell bladder carcinoma with very long-term catheterization (see also complications of Foley catheters).
| Foley catheter | Index | Intermittent catheter |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Gambrill B, Pertusati F, Hughes SF, Shergill I, Prokopovich P. Materials-based incidence of urinary catheter associated urinary tract infections and the causative micro-organisms: systematic review and meta-analysis. BMC Urol. 2024 Aug 30;24(1):186. doi: 10.1186/s12894-024-01565-x.
Robinson J. Urethral catheter selection. Nurs Stand. 2001 Mar 7-13;15(25):39-42. doi: 10.7748/ns2001.03.15.25.39.c2993.
Sökeland, J., Brühl, P., Hertle, L., and Piechota, H. (2000).
Katheterdrainage der Harnblase heute.
Dtsch Arztebl, 97(4):A167-A174.
 Deutsche Version: Indikationen und Legetechnik für suprapubischer Katheter
Deutsche Version: Indikationen und Legetechnik für suprapubischer Katheter
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.