You are here: Urology Textbook > Kidneys > Renal cell carcinoma > Diagnosis
Renal Cell Carcinoma: Symptoms and Diagnostic Workup
- Renal cell carcinoma: Definition and Epidemiology
- Renal cell carcinoma: Pathology
- Renal cell carcinoma: Diagnostic workup
- Renal cell carcinoma: Surgical Treatment
- Renal cell carcinoma: Targeted therapy of advanced disease
Signs and Symptoms of Renal Cell Carcinoma
Without symptoms:
Over 50% of RCC are discovered incidentally (widespread use of imaging) and are asymptomatic.
Classic triad of symptoms:
Advanced renal cell carcinoma symptoms are flank pain, hematuria, and palpable abdominal tumor.
B symptoms:
Night sweats, weight loss and fever are signs of a significant tumor burden.
Metastases:
Metastases may cause cough, shortness of breath, bone pain, neurological problems, and jaundice.
Paraneoplastic syndromes:
Up to 20% of renal cell carcinomas produce ectopic hormones and may present with paraneoplastic symptoms (Gold et al., 1996).
Hypercalcemia:
Hypercalcemia is caused by parathyroid hormone-like substances, vitamin D3, prostaglandins, or bone metastases.
Polycythemia and hypertension:
Renin or erythropoetin production.
Stauffer syndrome:
Stauffer syndrome is a reversible syndrome of hepatic dysfunction (elevated AP, bilirubin, and transaminases with pathological coagulation), which is probably triggered by cytokines (e.g., IL-6). Normalization may be expected in 70% after nephrectomy.
Further paraneoplastic symptoms:
Leukemoid reaction, thrombocytosis, Cushing syndrome, hirsutism, and gynecomastia.
Basic Investigations for Renal Tumor:
The following studies are always indicated for a suspected renal tumor (Riccabona et al., 2003):
- laboratory tests
- ultrasound imaging of the kidneys and liver
- Abdominal CT scan with contrast medium, alternatively MRT of the kidneys
- Chest X-ray p.a. and side view (alternatively CT thorax)
Laboratory tests:
- creatinine
- urine sediment
- complete blood count
- calcium
- liver enzymes
- AP, LDH
- blood clotting tests
Ultrasound Imaging:
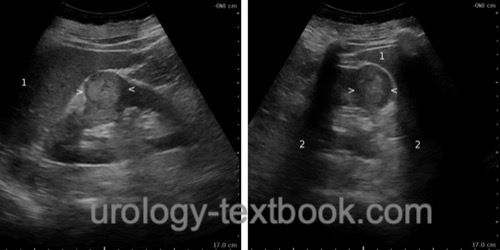
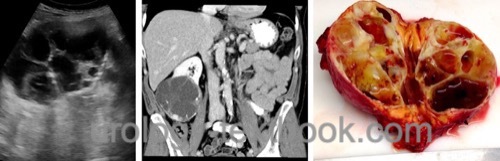
Renal cell cancer presents as mostly hypoechoic to isoechoic tumor in the kidney, growing in the center of the kidney or bulging into the perirenal fat [fig. ultrasound imaging of renal cell carcinoma]. Cystic tumors are difficult to assess in sonography [fig.~\ref {rcc_zystisch2}]. Lesions of the kidney suspicious of renal cell cancer are further investigated with abdominal computed tomography (with contrast medium) or alternatively with MRI of the kidney.
The liver should be examined for liver metastases. In advanced tumors, Doppler ultrasound imaging may reveal a thombus in the renal vein or vena cava inferior.
 |
 |
Abdominal Computed Tomography:
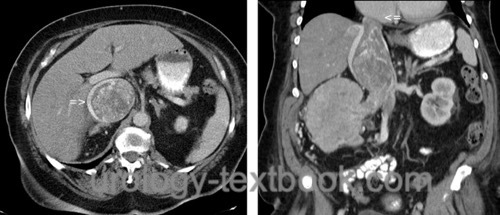
CT is the imaging technique of first choice for patients with suspected renal cell carcinoma to assess tumor stage and for planning surgical therapy [fig. renal cell carcinoma in CT]. The multiple planes of CT imaging help to assess the possibility of partial nephrectomy and to decide about open or laparoscopic surgical approach [fig. cystic renal cell carcinoma]. The cranial extent of a tumor thrombus can be determined [fig. large RCC with vena cava thrombus]. Lymph node enlargement of more than 1 cm is suspect for lymphonodular metastasis. In addition to preoperative staging, CT can estimate the renal function of the contralateral side.
 |
 |
 |
MR Imaging:
Cross-sectional imaging for patients with chronic kidney disease, with contraindications for iodinated contrast agents, inconclusive findings in CT, and suspected infiltration of neighboring organs. MRI (with imaging of the right atrium) is the best method for examining the cranial extent of a vena cava thrombus.
Chest X-Ray or CT-Thorax:
Chest X-ray is sufficient for patients with low risk for pulmonary metastasis. Chest CT is preferable for patients with larger tumors, symptomatic RCC, and if chest X-ray shows pathological findings.
Investigations Reserved for Special Situations:
Venography or transesophageal ultrasound:
Indicated for suspected cava thrombus and contraindication to MRI.
Whole-Body Low-Dose CT or bone scintigraphy:
Whole-Body Low-Dose CT or bone scintigraphy detects bone metastases, indicated for advanced tumors with elevated AP, bone pain, or metastases in other locations.
Brain MRI:
Initiate brain MRI if cerebral metastases are suspected.
Positron emission tomography:
PET has no proven benefit in the diagnosis of renal cell carcinoma. There is no recommendation in the current guidelines for use, even for patients with advanced tumors.
Fine needle biopsy:
Biopsy of renal masses is indicated if abscess, lymphoma, or metastasis are suspected or if a histological confirmation of an advanced tumor is needed for targeted therapy. False negative histology may occur in 5–15%. Complications of the biopsy are bleeding, infection, arteriovenous fistula or pneumothorax. Serious complications or tumor contamination of the needle tract are rare.
Genetic evaluation:
Genetic evaluation should be offered to patients under 46 years of age, with bilateral or multifocal tumors, patients with affected first-degree or second-degree relatives, or with relatives and histological characteristics for hereditary renal cell carcinoma (e.g., multifocal papillary histology, HLRCC syndrome, multifocal chromophobe histology, succinate dehydrogenase-deficient renal cell carcinoma).
Screening of Renal Cell Carcinoma
Screening (Early Detection) with imaging is not recommended for the general population due to the low specificity of imaging, the low incidence of renal cell carcinoma, and the high prevalence of benign kidney tumors. Screening is recommended for the following risk groups: patients with end-stage renal failure, tuberous sclerosis, von Hippel-Lindau disease, and cystic kidney diseases.
Differential Diagnosis of a Renal Mass
The compilation is modified from [Campbell 2007].
Inflammatory renal tumors:
Abscess, xanthogranulomatous pyelonephritis, infected renal cyst, tuberculosis, rheumatic diseases with granulomas
Renal tumors of mature renal parenchyma:
Adenoma, renal cell carcinoma.
Renal tumors of immature renal parenchyma:
Wilms tumor, sarcoma.
Renal tumors of the renal pelvis:
Papillomas, transitional cell carcinoma, squamous cell carcinoma, adenocarcinoma.
Cystic renal tumors:
Simple or complex renal cyst, parapelvic renal cysts, benign multilocular renal cyst, calyceal diverticula, cystic nephroma, polycystic kidney disease, Hippel-Lindau disease, tuberous sclerosis, lymph cysts.
Renal tumors of the vascular system:
Hemangioma, hamartoma, lymphangioma, angiomyolipoma.
Renal tumors of the nervous system:
Neuroblastoma, sympathicoblastoma, schwannoma.
Mesenchymal renal tumors:
Fibroma, fibrosarcoma, lipoma, liposarcoma, leiomyoma, leiomyosarcoma.
Perirenal renal tumors:
Retroperitoneal sarcoma and other mesenchymal tumors, teratoma, neuroblastoma, lymphoma, lymph node metastases of e.g., testicular tumors.
Renal metastases:
Lung cancer, breast cancer, gastrointestinal cancers, malignant melanoma, lymphoma.
| RCC symptoms | Index | RCC nephrectomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
 Deutsche Version: Nierenzellkarzinom
Deutsche Version: Nierenzellkarzinom
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.