You are here: Urology Textbook > Kidneys > Simple renal cyst
Simple Renal Cysts: Benign Lesions of the Kidney
Definition of a Simple Renal Cyst
Simple renal cysts occur unilateral or bilateral, single or multiple. Renal cysts are usually circular, filled with clear fluid, and have no connection to the pyelocalyceal system.
 |
Epidemiology
The prevalence rate of kidney cysts increases with age: 20% at 40 years and 33% at 60 years of age.
Etiology and Pathology of Kidney Cysts
Causes of simple renal cyst:
Simple renal cysts derive from a segment of the nephron.
Pathology of a simple renal cyst:
Simple renal cysts have a fibrous cyst wall lined with a simple flat to cuboidal epithelium.
Signs and Symptoms
Kidney cysts usually do not cause any symptoms. Simple kidney cysts may cause complications like:
- Abdominal or lumbar pain: due to the displacement of abdominal organs, rupture, or bleeding of the renal cyst.
- Hematuria: due to rupture of a renal cyst into the pyelocalyceal system.
- Arterial hypertension: by compression of the renal artery.
- Hydronephrosis: due to compression of the ureter or renal pelvis.
Simple or Complex Kidney Cyst: Diagnosis
Most important with imaging of renal cysts is the classification into simple (benign) or complex (potential malign) renal cysts.
Ultrasound Imaging:
Sonographic criteria for a simple renal cyst are:
- Round lesion of the kidney with echo-free content
- No septa
- No thickening of the round to oval cyst wall, no calcifications
- Posterior acoustic enhancement
Computed Tomography (CT)
CT imaging is indicated for suspicious ultrasound findings such as septation, clustering of cysts, wall thickening or calcification or echogenic contents of the cyst.
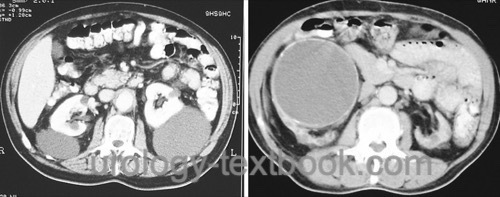
The criteria for a simple renal cyst in computed tomography are similar to the ultrasound (see above); the density is −10 to 20 HU. A simple hyperdense cyst with 20–90 HU is also possible. The most crucial criterion for a benign cyst is no enhancement of the cyst or the cyst wall after infusion of contrast medium. Calcifications are not obligate suspect [fig simple renal cysts].
Bosniak Classification of renal cystic masses (Israel and Bosniak, 2005):
- Bosniak I: clearly benign cyst. No risk of malignancy.
- Bosniak II: few thin (<1 mm) septa or thin calcifications (thickness not measurable), hyperdense lesions (due to proteinaceous or hemorrhagic contents) are non-enhancing after contrast medium infusion, size <3 cm. The risk of malignancy is 0%; follow-up is unnecessary.
- Bosniak IIF: this group subsumes cysts, which cannot be clearly assigned to Bosniak II or III. The risk of malignancy is 5%, and close follow-up is necessary (the 'F' in 2F is for 'follow').
- Bosniak III: not clearly benign cyst: wall or septa with more than 1 mm thickness and measurable enhancement. Surgical excision is necessary, and the risk of malignancy is 50%.
- Bosniak IV: cyst with clear malign criteria; partial nephrectomy or radical nephrectomy is necessary. The risk of malignancy is 75–90%.
Contrast-enhanced ultrasound imaging:
CEUS can improve the diagnostic value of ultrasound imaging (operator-dependent) and may reduce the need for CT for suspicious cysts.
Magnetic Resonance Imaging (MRI)
MRI is a good alternative to computed tomography, especially when follow-up of suspicious lesions is required. MRI avoids the high radiation exposure of a multiphase ct examination and provides higher soft-tissue contrast with better differentiation of hemorrhagic or lipomatous components. Patient cooperation during the examination is important to minimize artifacts caused by respiratory motion of the kidneys.
Treatment of Simple Renal Cysts
Percutaneous Puncture and Aspiration of Renal Cysts
Pain due to a kidney cyst should disappear after diagnostic puncture and aspiration, at least for a while. A single puncture and aspiration cure a small proportion of patients. In addition, the cyst fluid is examined (cytology and creatinine concentration). A simple renal cyst should not reveal malignant cells; the creatinine concentration is near the serum concentration. If the cyst (and symptoms) recur, definitive treatment is possible with a percutaneous or laparoscopic approach (see below).
Percutaneous Sclerotherapy of Renal Cysts
A thin nephrostomy tube is placed into the renal cyst with ultrasound guidance. As described above, the cyst volume and creatinine concentration is measured. The creatinine concentration should be near the serum concentration. Consider a cytological investigation to exclude malignancy.
Before sclerotherapy, contrast medium is injected via the nephrostomy tube into the cyst. The contrast medium should not enter the pyelocalyceal system. The most commonly used sclerosant is ethanol (99%); the dosage is 20% of the cyst volume to a maximum of 100 ml. The alcohol is left 90–120 min in the cyst: the longer the alcohol contact (several fillings, contact time), the lower the recurrence rate. An alternative sclerosant is polidocanol. A relapse of the cyst occurs in approximately 10–30%. Percutaneous sclerotherapy can be repeated.
Laparoscopic Deroofing of Kidney Cysts
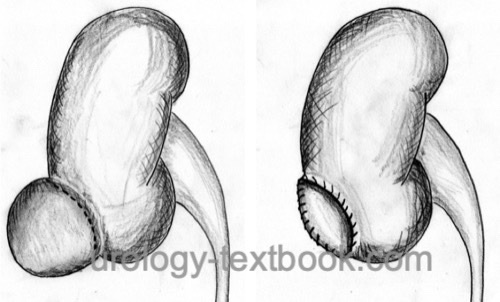
The laparoscopic or retroperitoneoscopic approach is the preferred technique. If the cyst is in anatomic proximity to the ureter, the ureter has to be identified and separated from the cyst wall. The cyst wall is circularly incised near the renal parenchyma (deroofing). The base of the cyst remains in situ. The cyst roof is sent for pathology. Hemostasis is essential and achieved with bipolar cauterization or continuous stitching of the remaining cyst wall. Laparoscopic cyst deroofing is used for very large renal cysts [fig.~\ref{lap_nierenzyste}].
 |
Prognosis of Simple Kidney Cysts
25% of kidney cysts show a trend of enlargement within three years. See above (Bosniak classification) for malignancy risk.
| Multilocular cyst | Index | Parapelvic cysts |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Israel, G. M. & Bosniak, M. A.
An update of the Bosniak renal cyst classification system.
Urology, 2005, 66, 484-488
 Deutsche Version: Nierenzyste
Deutsche Version: Nierenzyste
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.