You are here: Urology Textbook > Kidneys > Kidney transplantation
Kidney Transplantation: Indications, Technique, and Prognosis
Kidney transplantation is a renal replacement therapy for patients with end-stage renal failure, which improves survival and quality of life compared to hemodialysis (Halloran, 2004) (Perico et al., 2004). EAU guidelines kidney transplantation.
 |
Epidemiology
Prevalence of kidney transplantation:
Approximately 27% of end-stage renal failure patients in Germany are treated by renal transplantation; this corresponds to a prevalence in the general population of roughly 30 per 100,000. The figures in the USA are comparable (30% of end-stage renal failure patients are treated by renal transplantation).
Etiology of End-Stage Renal Failure
See section chronic kidney disease.
Contraindications to Kidney Transplantation
Infections:
Acute or chronic bacterial or viral infections, chronic periodontitis, diverticulitis, cholecystitis, HIV (changing), chronic pyelonephritis (nephrectomy necessary), and active chronic hepatitis.
Cancer:
Depending on the tumor stage, a disease-free interval of at least two years is required. Metastases are an absolute contraindication.
Systemic diseases:
Advanced heart, lung, or liver insufficiency.
Positive cross-matching test:
Detection of transplant-relevant circulating antibodies in the recipient directed against donor antigens.
Indication for nephrectomy before transplantation:
Severe renal arterial hypertension, chronic pyelonephritis (with or without VUR), pronounced proteinuria, symptomatic polycystic kidneys, enlarged polycystic kidneys (extend below iliac crest), nephrolithiasis, and kidney tumors.
Living-Donor Kidney Transplantation
Conditions for living-donor kidney transplantation:
The recipient must be suitable and listed for kidney transplantation. A commercial donation must be excluded, as must the donor's psychological dependence on the recipient. In Germany, it is prohibited by law to donate organs to strangers.
Good health and two healthy kidneys in the donor are indispensable requirements. See the following table for the diagnostic workup of the donor:
| Diagnostic workup | |
| Urine tests | Exclusion of urinary tract infection, proteinuria and hematuria in 24-hours urine collection. |
| Laboratory tests | Thorough routine laboratory tests including glucose tolerance test, blood group antigens, cross-matching, serology of HIV, HCV, HBV, CMV, EBV, syphilis, toxoplasmosis. |
| Medical evaluation | Exclusion of significant medical diseases such as cardiovascular diseases, lung diseases, diabetes mellitus, tumors, or chronic infections. |
| Urological evaluation | Exclusion of recurrent UTI, nephrolithiasis, micturition disorders, hematuria and tumors. MRI or spiral CT angiography to assess the anatomy and to exclude diseases of the urogenital tract, and split renal function by scintigraphy. |
For contraindications to living donation see the following table:
| Absolute Contraindikations |
| Age under 18 years (e.g. Germany) |
| Diabetes mellitus |
| Uncontrolled arterial hypertension |
| Proteinuria (>300 mg/24 h) |
| GFR below 70 ml/min/1,75 m2 |
| Nephrolithiasis with risk of recurrence |
| Increased risk of thromboembolism |
| Signifikant medical diseases |
| BMI >35 kg/m2 |
| HIV infection |
| Pregnancy |
| Tumor diseases with a disease-free interval <5–10 Jahre |
| Relative Contraindikations |
| Chronic infections (Tbc, Hep B/C) |
| BMI >30 kg/m2 |
| Mental illness |
| Microhematuria without visible kidney disease |
The weaker kidney of the donor is always used for a living donation. A negative cross-matching test between donor and recipient is mandatory. Concerning blood group antigens, blood group compatibility is sufficient for kidney donation, see the following table.
| Recipient | Possible Donor |
| 0 | 0 |
| A | A and 0 |
| B | B und 0 |
| AB | A, B, AB and 0 |
There are protocols for enhanced immunosuppression for AB0 incompatible kidney transplants or HLA donor-specific antibodies, but graft survival is inferior. To enable more living-donor kidney transplantation between AB0-incompatible donors and recipients, kidney paired donation or other kidney exchange programs across a region is a solution. Kidney paired donation is prohibited by law in Germany.
Donor risks of live kidney donation:
Mortality 0.03–0.06%, serious complications 2–4%. A total of up to 30% complications, most often pneumonia, urinary tract infection, wound infection, pneumothorax, ileus, hematoma, incisional hernia, prolonged pain, thrombosis and embolism (Kasiske et al., 1996).
Technique of donor nephrectomy:
Open, laparoscopic or retroperitoneoscopic approach. Careful preparation of the renal vessels to preserve adequate length. Dissect the ureter well below the iliac vessels. Dissect the renal vessels with a vascular stapling device and perform organ removal. Further preparation of the organ after perfusion with cold organ preservation solution ex-situ.
Deceased-Donor Kidney Transplantation
Prerequisites for organ removal in Germany:
Consent for organ donation by the patient (organ donation card) or relatives. Two independent doctors have confirmed donor death: brain death without brain stem reflexes.
Organ donation after cardiac death:
In some countries (UK, Switzerland, Netherlands, Spain, Belgium, and the USA), a cardiac and circulatory arrest of 10 min at normal body temperature is sufficient for the final diagnosis of death, after which brain function is considered irretrievably lost. Kidney donation from "non-heart-beating donors (NHBD)" is successful within 60–120 min; the long-term results are comparable to organ donation after brain death. In Germany, the transplantation of organs after cardiac death is not allowed due to ethical considerations and the risk of misdiagnosis (Weiller et al., 2014).
Contraindications of the donor:
Uncontrolled cancer, infections (hepatitis, HIV, tuberculosis, sepsis, drug abuse). Insufficient kidney function: serum creatinine should be below 2 mg/dl.
Selection of the recipient:
Suitable recipients in Central Europe are selected by Eurotransplant in Leiden (Netherlands). Selection criteria are AB0 system, HLA antigens, waiting time, age of donor and recipient, and urgency. Eurotransplant cooperates with other comparable organizations in Europe. This enables the optimal distribution of the available organs based on biochemical properties and improves graft survival despite longer preservation times due to transport. If the organ quality of a single kidney is judged to be too poor, the option of dual kidney transplantation exists: two kidneys are transplanted together.
Kidney Donor Profile Index (KDPI):
KDPI describes the organ quality of the donor and correlates with graft survival; factors used are age, height, weight, ethnicity, arterial hypertension, diabetes, cause of death, serum creatinine, hepatitis C status, and donation after cardiac death. The KDPI is used for distribution in the U.S.: very good donor kidneys are distributed to patients with long life expectancy; organs with a poor KDPI are still a good option for older comorbid patients.
Donor kidney biopsy:
A donor kidney biopsy can assess organ quality before transplantation and is regularly performed in the USA. Indications are donors with a risk for renal dysfunction like anuria, creatinine over 1.5 mg/dl, diabetes mellitus, KDPI over 85%, or age over 60 years. Problematic are the time constraints of organ allocation, the inconsistent assessment of histological lesions and the inaccuracy (frozen section, lack of experience of the on-call pathologist). Procurement biopsy findings are the most common cause of kidney discard in the USA.
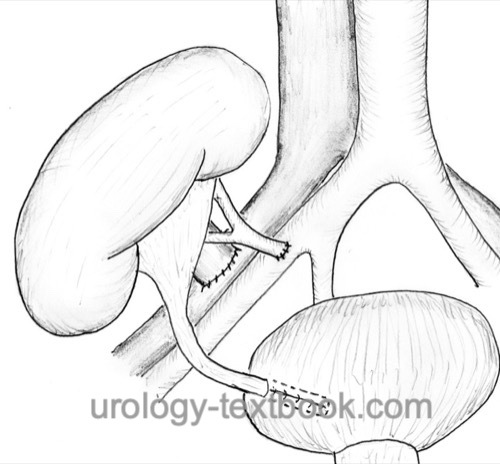
Surgical technique of kidney transplantation:
Retroperitoneal surgical access to the iliac vessels via a pararectal or Gibson incision. Careful handling and sparing of the lymphatic vessels. The left kidney is usually anastomosed with the right iliac vessels and vice versa [fig. kidney transplantation]. The vein is anastomosed before the artery. The external or common iliac artery and vein are usually used for anastomosis (end-to-side). The ureter is implanted with an extravesical antirefluxing ureterocystoneostomy (Lich-Gregoir techniques) with a short DJ stent.
Complications of Kidney Transplantation:
Hemorrhage, wound infection, arterial or venous thrombosis of the graft with loss of function, lymphocele, urinoma, ureteral stenosis, vesicoureteral reflux, pyelonephritis, kidney stones, hyperacute, active or chronic rejection (T-cell or antibody mediated).
Immunosuppression After Kidney Transplantation
In principle, the following substance groups are used for immunosuppression after kidney transplantation:
- Glucocorticoids
- Calcineurin inhibitors: ciclosporin, tacrolimus
- mTOR inhibitors: sirolimus, everolimus
- Purine synthesis (IMPDH) inhibitors: mycophenolate-mofetil
- Antimetabolites: azathioprine
- Antibodies against T and B lymphocytes: Lymphocyte-decimating antibodies (antithymocyte globulin), monoclonal anti-CD3 AK (Muromonab-CD3), monoclonal anti-CD52 AK (alemtuzumab), monoclonal anti-CD25 AK (daclizumab, basiliximab) and monoclonal anti-CD20 AK (rituximab).
Immunosuppression protocols:
Immunosuppression protocols are divided into the following phases:
Induction therapy:
Immunosuppressive therapy before transplantation, e.g., plasmapheresis for the elimination of circulating antibodies or the administration of antibodies against immune cells.
Initial immunosuppression:
Up to three months after renal transplantation, combinations of a calcineurin inhibitor (ciclosporin or tacrolimus), combined with mycophenolate mofetil and glucocorticoids. Alternatives are combination therapies with mTOR inhibitors.
Additional administration of antibodies against immune cells is optional and recommended in patients with delayed graft function or a high risk of rejection (HLA antibodies).
Maintenance therapy:
The immunosuppression is reduced: calcineurin inhibitors, combined with azathioprine or mycophenolate mofetil and low-dose glucocorticoids are used. Rejection is treated with high-dose steroids or antibodies against immune cells.
Modifications:
There are numerous modifications of the traditional protocol: without steroids, without cyclosporin or strong induction therapy with minimal immunosuppression thereafter.
Prognosis
- Living donor kidney transplantation: 1- and 10-year graft survival rate in unrelated donors is 92% and 56%.
- Deceased donor kidney transplantation: 1- and 10-year graft survival rate is 87% and 50%.
| Dialysis | Index | Oncocytoma |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Breda, A.; Olsburgh, J.; Budde, K.; Figueiredo,
A.; Lledó García, L. & Regele, H.
EAU Guideline: Renal
Transplantation
2019. https://uroweb.org/guidelines/renal-transplantation/
BTS & Renal Association UK Guidelines for living donor kidney transplantation, online abgerufen auf http://www.cambridge-transplant.org.uk/program/renal/lrdgui.pdf am 22.2.2011.
Halloran 2004 HALLORAN, P. F.:
Immunosuppressive drugs for kidney transplantation.
In: N Engl J Med
351 (2004), Nr. 26, S. 2715–29
Perico u.a. 2004 PERICO, N. ; CATTANEO, D. ;
SAYEGH, M. H. ; REMUZZI, G.:
Delayed graft function in kidney transplantation.
In: Lancet
364 (2004), Nr. 9447, S. 1814–27
 Deutsche Version: Indikationen und Technik der Nierentransplantation
Deutsche Version: Indikationen und Technik der Nierentransplantation
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.