You are here: Urology Textbook > Surgery (procedures) > Ureterocystoneostomy
Ureterocystoneostomy: Leadbetter, Cohen and Lich-Gregoir Technique
Transvesical Ureterocystoneostomy
Ureterocystoneostomy is the reimplantation of the ureter into the bladder and is used for treatment of vesicoureteral reflux (VUR). In the transvesical technique, the distal ureter is mobilized after opening the urinary bladder and reimplanted into a submucosal neotunnel (Steffens et al., 2006).
- Leadbetter-Politano technique: the neotunnel is created above the ureteral orifice, which remains the same place.
- Cohen technique: the neotunnel is created in extension of the ureteral course, the ureteral orifice is shifted to the opposite side of the trigonum (transtrigonal reimplantation)
 |
Contraindications
- Coagulation disorders.
- Kidneys without sufficient function (<15% of total glomerular filtration rate)
- High surgical risk due to the comorbidity of the patient.
Surgical Technique of Transvesical Ureterocystoneostomy
Preoperative Patient Preparation
- Cystoscopy, retrograde pyelography and VCUG to confirm the diagnosis.
- Exclude or treat urinary tract infections
- Perioperative antibiotic prophylaxis
- Transurethral bladder catheter after disinfection and sterile draping.
Surgical Approach
A Pfannenstiel incision is sufficient to treat VUR in children. Fat is removed from the anterior wall of the bladder and disturbing blood vessels are coagulated. Place stay sutures and open the bladder vertically.
Leadbetter-Politano Reimplantation:
- Insert a MJ splint and fix it with thin rapidly absorbable suture to the ureteral orifice. Circumcise the ureteral orifice, dissect the intramural part of the ureter with fine scissors under light traction with the splint.
- Fully mobilize the distal ureter and proceed with additional extravesical preparation as far as possible.
- Use a right-angle clamp to perforate the bladder 3--4~cm cranial of the old orifice for the neo-hiatus and secure the new passage with a vessel loop.
- Pass the ureter including splint through the neo-hiatus and close the old hiatus with PDS 4-0.
- A submucosal tunnel is created between the neo-hiatus and the old orifice.
- Pass the ureter including splint through the neo-hiatus. Resect and spatulate the dysplastic part of the distal ureter. Anchor the ureter to the mucosa of the old ostium with PDS 4-0. At 6 o'clock, place deep sutures with the muscularis of the urinary bladder for secure fixation.
- Close the mucosal defect at the neo-hiatus.
- For uncomplicated surgery, some authors remove the ureteral stent. Alternatively, insert a new ureteral stent or feeding tube 4–5 CH for security and to check the width and lack of kinking. Exit the ureteral splint through a separate stab incision of bladder and skin.
- Place a Suprapubic catheter, a drainage if needed, and close the bladder in two layers.
Cohen Reimplantation:
After transvesical mobilization of the ureter, a submucosal tunnel is created in direction of the oppposite ureteral orifice. Pass the ureter including stent through the neotunnel to the new ostium and anchor like described above. The Cohen technique is considered easier as the ureter does not have to be repositioned. However, endoscopic interventions of the upper urinary tract (e.g., ureterorenoscopy) in the further course of life are difficult and a significant disadvantage.
Technical Modifications:
The Leadbetter and Cohen technique can be performed vesicoscopically (endoscopic robotic-assisted), series with small numbers have been published (Kruppa et al., 2023).
Postoperative Care after Transvesical Ureterocystoneostomy
General Measures:
Early mobilization, thrombosis prophylaxis depending on age, laboratory tests (hemoglobin, creatinine), regular physical examination of the abdomen and incision wound.
Analgesia:
Analgesics with a combination of NSAIDs and opioids.
Drains and Catheters:
Quickly remove the transurethral catheter depending on hematuria. Remove the pelvic drain if the daily drainage volume is below 50 ml. The ureteral splint can be removed after 5–7 days. Suprapubic catheter 8–10 days, a cystography is usually not necessary.
Complications of Transvesical Ureterocystoneostomy
- Hydronephrosis: postoperative hydronephrosis often improves spontaneously after resolution of the postoperative edema and hematoma. The (re)insertion of a ureteral stent is technically difficult (alternative: percutaneous nephrostomy). In rare cases, scarring, kinking of the ureter or ischemia can lead to a ureteral stricture and necessitate surgical revision.
- Further complications: (persistent) vesicoureteral reflux, hemorrhage, wound infection, urinary tract infections, urinoma. Injury of the vas deferens.
Extravesical Lich-Gregoir Ureterocystoneostomy
Ureterocystoneostomy is the reimplantation of the ureter into the bladder and is used for treatment of vesicoureteral reflux (VUR). In the extravesical Lich-Gregoir technique, the intramural ureter is dissected extravesically from the dorsal side without opening the bladder (Riedmiller et al., 2008). Tunneling is achieved by incision and closure of the bladder wall above the ureter.
Contraindications
- Coagulation disorders.
- Kidneys without sufficient function (<15% of total glomerular filtration rate)
- High surgical risk due to the comorbidity of the patient.
- Intravesical pathology such as ureterocele, megaureter, or ectopic ureter.
- Infants in the first 12 months of life or adults.
Surgical Technique of Extravesical Lich-Gregoir Ureteral Reimplantation
Preoperative Patient Preparation
- Cystoscopy, retrograde pyelography and VCUG to confirm the diagnosis.
- Exclude or treat urinary tract infections
- Perioperative antibiotic prophylaxis
- Transurethral bladder catheter after disinfection and sterile draping. Fill the bladder
Surgical Approach
A Pfannenstiel incision is sufficient to treat VUR in children. The urinary bladder is exposed extraperitoneally; the ureter is identified under the medial umbilical ligament (after transection) and marked with a vessel loop.
Lich-Gregoir Reimplantation:
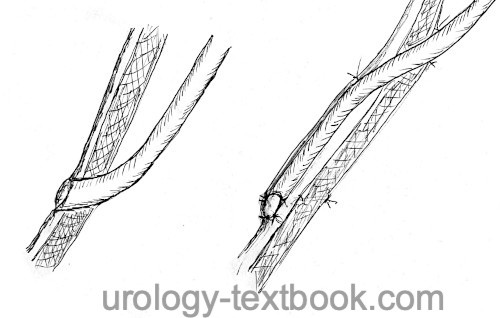
A submucosal tunnel is achieved by incision of the detrusor (detrusortomy) and closure over the ureter.
- The detrusortomy starts at the ureteral orifice and is directed 4–5 cm along the natural course of the ureter.
- Create more space for the submucosal tunnel by blunt and sharp dissection between detrusor and mucosa.
- The ureter is placed in the detrusortomy, which is closed with interrupted 4-0 absorbable monofilament sutures. The ureter is now in a long submucosal position preventing reflux.
- Place a Suprapubic catheter, a drainage if needed, and close the bladder in two layers.
Technical Modifications:
The Lich-Gregoir technique can be performed laparoscopically (robotic-assisted) with excellent vision (Weiss et al., 2015).
Postoperative Care after Lich-Gregoir Ureterocystoneostomy
General Measures:
Early mobilization, thrombosis prophylaxis depending on age, laboratory tests (hemoglobin, creatinine), regular physical examination of the abdomen and incision wound.
Analgesia:
Analgesics with a combination of NSAIDs and opioids.
Catheter:
Quickly remove the transurethral catheter depending on hematuria and possible injury of the mucosa. Control for residual voiding volume.
Complications of Transvesical Ureterocystoneostomy
- Postvoid residual urine: after bilateral Lich-Gregoir surgery, up to 10% develop a temporary bladder emptying disorder. The bilateral nerve injury in the area of the trigonum causes the high rate of bladder voiding dysfunction.
- Hydronephrosis: postoperative hydronephrosis often improves spontaneously after resolution of the postoperative edema and hematoma. The (re)insertion of a ureteral stent is technically difficult (alternative: nephrostomy). In rare cases, scarring, kinking of the ureter or ischemia can lead to a ureteral stricture and necessitate surgical revision.
- Further complications: (persistent) vesicoureteral reflux, hemorrhage, wound infection, urinary tract infections, urinoma. Injury of the vas deferens.
| Transureteroureterostomy | Index | Ureteral reimplantation: Psoas hitch and Boari flap |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Hinman: Atlas Urologischer Operationen im Kindes- und Erwachsenenalter.
C. Kruppa et al., “Vesicoscopic vs. Open Ureteral Reimplantation According to Cohen and Leadbetter-Politano for Vesicoureteral Reflux.,” J Clin Med., vol. 12, no. 17, 2023, doi: 10.3390/jcm12175686.
H. Riedmiller and E. W. Gerharz, “Antireflux surgery: Lich-Gregoir extravesical ureteric tunnelling.,” BJU int., vol. 101, no. 11, pp. 1467–1482, 2008, doi: 10.1111/j.1464-410X.2008.07683.x.
J. Steffens, E. Stark, B. Haben, and A. Treiyer, “Politano-Leadbetter ureteric reimplantation.,” BJU int., vol. 98, no. 3, pp. 695–712, 2006, doi: 10.1111/j.1464-410X.2006.06407.x.
 Deutsche Version: Harnleiterreimplantation: Technik nach Leadbetter, Lich-Gregoir, Psoas hitch und Boari Lappen
Deutsche Version: Harnleiterreimplantation: Technik nach Leadbetter, Lich-Gregoir, Psoas hitch und Boari Lappen
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.