You are here: Urology Textbook > Penis > Priapism
Priapism: Definition, Diagnosis, and Treatment
Definition of Priapism
Priapism is an unwanted persisting penile erection that lasts at least two hours without sexual stimulation and is associated with the risk of erectile tissue damage.
The name priapism is derived from Priapus, the Greek god of fertility.
Epidemiology of Priapism
The incidence of priapism is about 1–3/100 000. Intracavernosal pharmacotherapy and sickle cell disease are important risk factors. Age groups at particular risk are children between 5–10 years (sickle cell disease) and men between 20–50 years (medication and drugs), but priapism can be possible at any age.
Causes (Etiology) of Priapism
Idiopathic Priapism (30%):
The failure of the physiological detumescence is unclear.
Priapism Induced by Medication and Drugs (20%):
Cocaine, alcohol, painkillers, psychiatric drugs, anesthetics, anticonvulsants, or antihypertensives may cause priapism. The antagonism of α1-receptors prevents the smooth muscle contraction of the erectile tissue and, thus, the detumescence. Phosphodiesterase inhibitors are only a rare cause of priapism.
Sickle Cell disease (10–20%):
A vaso-occlusive crisis is caused by sickling of the red blood cells; the crisis is induced by manipulation or nocturnal hypoventilation and results in a decreased venous outflow and ischemic priapism. Ischemia increases the sickling of the red blood cells and worsens the impaired venous outflow. The lifelong risk in homozygous sickle cell disease of suffering a priapism is 40–90%.
Intracavernous Pharmacotherapy:
Older preparations of intracavernous pharmacotherapy, such as papaverine (opium alkaloid) and phentolamine (alpha Blocker), cause more often priapism than pharmacotherapy with prostaglandin E1. About 1% of men treated with prostaglandin E1 experience priapism.
Neurological diseases:
Spinal cord compression (lumbar stenosis, herniated disc) or rarely spinal anesthesia can cause priapism.
Malignant Neoplasms:
Tumor infiltration in penile veins may rarely cause priapism. Tumors causing priapism are leukemia, prostate cancer, renal cell carcinoma, melanoma, and inflammatory pelvic tumors.
Priapism due to Trauma:
A blunt perineal trauma or puncture of the erectile tissue may cause injury to arteries in the corpus cavernosum. The increase of arterial flow may exceed the venous capacities, and a non-ischemic priapism may result.
Rare Causes of Priapism:
Long-lasting sexual activity, insect bites, parenteral nutrition (caused by fast infusion of highly concentrated fat).
Pathophysiology and Clinical Manifestations of Priapism
Ischemic (Low-Flow) Priapism
The failure of the physiological detumescence causes the persistence of the erection, which is tight and painful. The pressure within the erectile tissue is higher than the diastolic blood pressure (80–120 mmHg), and insufficient blood flow leads to ischemia. Ischemia causes paralysis of the smooth muscle cells in the erectile tissue and creates a vicious circle. The high fibrinolytic activity in the erectile tissue prevents the formation of thrombi. An irreversible damage of the erectile tissue with fibrotic healing is probable after 12 hours of ischemic priapism.
Non-ischemic (High-Flow) Priapism
The increased arterial inflow is higher than the maximum venous outflow. There is no risk of ischemic damage to the erectile tissue. The erection in non-ischemic priapism is less tense and less painful.
Diagnostic Workup of Priapism
Laboratory Tests:
- Complete blood count
- Hemoglobin S to exclude sickle cell disease
- Drug screening, if reasonable
Cavernous Aspiration with Blood Gas Sampling:
Blood gas testing with aspirated blood from the corpus cavernosum is essential to differentiate between high- or low-flow priapism using oxygen concentration, carbon dioxide concentration, and acidosis. High-flow priapism will likely show arterial blood gas values (pO2 >70 mmHg, no acidosis, pCO2 <50 mmHg). Patients with low-flow priapism typically have venous or ischemic blood gas values (pO2 <40 mmHg, acidosis, pCO2 >60 mmHg).
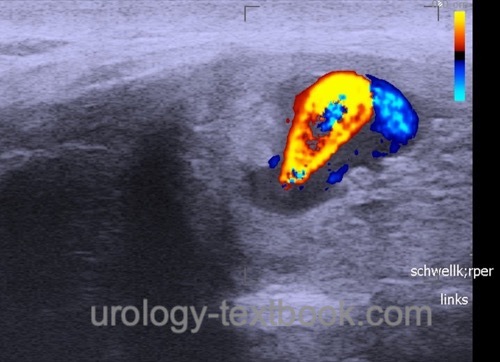
Doppler-Ultrasound of the Penis:
- Ischemic (low-flow) priapism reveals a low arterial flow.
- Non-ischemic (high flow) priapism presents with an irregular high flow in the area of injury and a high venous outflow.
 |
Treatment of Priapism
Therapeutic Blood Aspiration:
After blood gas sampling to differentiate between low-flow and high-flow priapism, further aspiration of blood allows the injection of drugs with α-adrenergic activity (see below).
α-adrenergic Drugs:
After therapeutic blood aspiration, fractional intracavernosal injection of α-adrenergic drugs, e.g., highly diluted epinephrine or norepinephrine, are done to promote smooth muscle contraction. See table Dosage of intracavernosal injection for single dosage. Control of the arterial blood pressure is essential; repeated injections are possible if no hypertension is present. After incomplete detumescence, cooling and intermittent compression of the penis with a child's blood pressure cuff may improve the clinical situation.
Additional Treatment of Priapism in Sickle Cell Disease:
- Administration of oxygen
- Aggressive hyperhydration and metabolic alkalinization to avoid further sickling of blood cells
Surgical Treatment of Ischemic Priapism:
If conservative treatment of ischemic priapism fails, a surgical shunt between the corpus spongiosum and corpus cavernosum is necessary immediately.
Winter shunt:
A Winter shunt is technically easy and has a high success rate. Puncture of the corpus cavernosum (both sides) through the glans with a thick peripheral venous catheter or biopsy true-cut needle leads to a temporary shunt. Aspiration of the blood and flushing of the corpus cavernosum with alpha-adrenergic agonists is also possible (Winter, 1976).
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Ebbehoj shunt:
Analogous to the Winter shunt, a scalpel stitch opens the corpus cavernosum through the glans on either side. The glans is closed with a thin monofilament suture (Ebbehoj, 1974).
Al-Ghorab shunt:
Do a transverse incision of the glans distal to the sulcus. A circular incision of the tunica albuginea of the corpora cavernosa is done. Close the glans incision with thin monofilament sutures (Ercole and others, 1981).
Bulbar cavernospongiosal shunt:
Last resort if distal shunting fails. Exposure of the bulbar corpus spongiosum and corpus cavernosum. Bilateral side-to-side anastomosis after oval excision of the tunica albuginea of the two corpora.
Treatment of High-Flow Priapism:
Spontaneous resolution of high-flow priapism is likely (60%); ice packs may help in spontaneous thrombosis of the ruptured artery. If conservative treatment fails, selective embolization is the next step. The last treatment option is the surgical ligation of the ruptured artery, which can be identified with intraoperative Doppler ultrasonography.
Prognosis after Priapism
Erectile dysfunction in up to 50–90% if surgical treatment is necessary. Rarely does a syndrome of recurrent low-flow priapism evolve, which is explained by endothelial changes.
| Peyronie disease | Index | Phimosis |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
T. J. Bivalacqua, B. K. Allen, and G. B. Brock et al., “Diagnosis and Management of Priapism: AUA/SMSNA Guideline,” 2022. [Online]. Available: https://www.auanet.org/guidelines-and-quality/guidelines/diagnosis-and-management-of-priapism-aua/smsna-guideline-(2022).
EAU-Guidelines: Sexual and Reproductive Health
Ebbehoj 1974 EBBEHOJ, J.:
A new operation for priapism.
In: Scand J Plast Reconstr Surg
8 (1974), Nr. 3, S. 241–2
Ercole u.a. 1981 ERCOLE, C. J. ; PONTES,
J. E. ; PIERCE, Jr.:
Changing surgical concepts in the treatment of priapism.
In: J Urol
125 (1981), Nr. 2, S. 210–1
Melman und Serels 2000 MELMAN, A. ; SERELS, S.:
Priapism.
In: Int J Impot Res
12 Suppl 4 (2000), S. S133–9
Winter 1976 WINTER, C. C.:
Cure of idiopathic priapism: new procedure for creating fistula
between glans penis and corpora cavernosa.
In: Urology
8 (1976), Nr. 4, S. 389–91
 Deutsche Version: Priapismus
Deutsche Version: Priapismus
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.