You are here: Urology Textbook > Surgery (procedures) > Laparoscopic pelvic lymphadenectomy
Surgical Steps and Complications of Laparoscopic Pelvic Lymphadenectomy
Indications for Laparoscopic Pelvic Lymphadenectomy
- Localized prostate cancer, together with laparoscopic (robot-assisted) prostatectomy
- Localized prostate cancer with intermediate or high risk before perineal prostatectomy or curative radiotherapy. Surgical staging has been almost completely replaced by modern nuclear medicine imaging (PSMA-PET).
- Penile carcinoma with inguinal lymph node metastases (more than two affected lymph nodes or extracapsular growth)
Contraindications
Coagulation disorders. Do not perform lymphadenectomy for low-risk prostate cancer (PSA <10 ng/ml and Gleason sum <7), the risk for metastasis is too low. For any comorbidity with an increase in surgical risk, the indication of lymphadenectomy should be critically questioned, as it is a diagnostic procedure. Alternatively, PSMA-PET can be used to detect lymph node metastases.
Surgical Technique (Step by Step) of Laparoscopic Pelvic Lymphadenectomy
Preoperative Preparations:
- Recommend a low fiber diet two days before surgery and a clear liquid diet on the preoperative day to improve the intraabdominal space.
- Administer an enema the night before surgery.
- Perioperative placement of a urinary catheter and gastric tube.
- Perioperative antibiotic prophylaxis is needed if risk factors for surgical site infections are present.
Surgical Approach Via Laparoscopy
Patient Positioning:
Supine position with slight lumbar hyperextension. Secure fixation by belt over the chest, pelvis and calves with the arms resting next to the body, a steep Trendelenburg positioning should be possible. Disinfection and sterile draping of the abdomen.
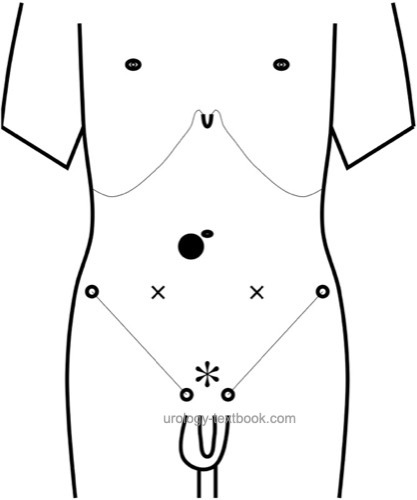
Trocar positions:
Create a Pneumoperitoneum with a mini-laparotomy or with the Veress needle next to the umbilicus (camera trocar 10 mm). Move the patient in Trendelenburg positioning after creation of a pneumoperitoneum. Place a 10 mm port suprasymphysary and two 5 mm ports lateral to the camera port, the trocars form a rhombus [see figure below]. Avoid injury to the epigastric vessels with transillumination.
 |
Lymphadenectomy of the right side:
Mobilize the caecum and appendix. Incise the parietal peritoneum along the external iliac artery from the iliac bifurcation to the internal inguinal ring. Incise the perivesicular tissue (periadventitia) over the external iliac artery, the lymphatic tissue over the artery and vein can be pushed medially with the dissection swab. Spare the lymphatic vessels from the lower extremity over or lateral to the external iliac artery. Expose the medial edge of the external iliac vein from the bifurcation to the pubic bone. Clip the lymphatic vessel of the mobilized package at the cranial and caudal border and harvest the package of the external iliac lymph nodes using a specimen bag.
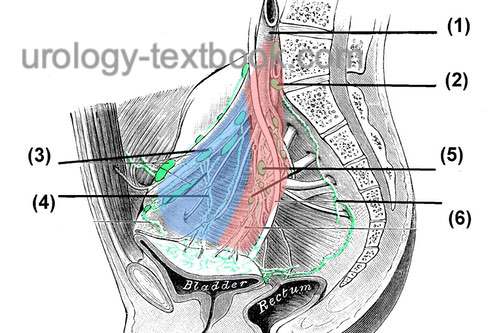 |
The next step includes the mobilization of the lymphatic tissue in the obturator fossa under the external ilical vein. Identify the obturator vessels and nerve below the lymphatic tissue for the dorsal border of the template. Caudally, the superior ramus of the os pubis is exposed, and the lymphatic vessels are clipped and transected. The lymphatic tissue of the fossa is traced cranially under the external iliac vein as far as possible, lymphatic vessels clipped and transected. Collect the obturatoric lymph nodes with a grasper and place them in the specimen bag [fig. lap. pelvic lymphadenectomy]. The lymph nodes along the internal iliac artery are dissected and harvested individually, and the medial border of the template is defined by the obliterated umbilical artery.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Lymphadenectomy of the left side:
Mobilize the sigmoid colon until the dissection area can be seen along the pelvic vascular axis. Incise the parietal peritoneum along the external iliac artery from the iliac bifurcation to the internal inguinal ring. Lymphadenectomy is performed as described on the right side. A drainage is unnecessary after transperitoneal surgery.
Postoperative Care
Early mobilization, thrombosis prophylaxis depending on risk factors and postoperative course, heparin injections above the navel. Laboratory checks (Hb), wound checks, abdominal examination and sonography of the lower abdomen to rule out lymphoceles.
Complications
Rare overall, possible complications include vascular injury with severe bleeding, nerve injury, lymphocele, bowel injury, ileus, peritonitis, ureteral injury, thrombosis, and pulmonary embolism.
| Retropubic radical prostatectomy | Index | Laparoscopic (robotic-assisted) radical prostatectomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
 Deutsche Version: Laparoskopische pelvine Lymphadenektomie
Deutsche Version: Laparoskopische pelvine Lymphadenektomie
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.