You are here: Urology Textbook > Surgery (procedures) > Vasectomy
No-Scalpel Vasectomy: Surgical Technique and Complications
Indications for Vasectomy
A vasectomy is a surgical procedure to sterilize a man, which is often used as a permanent method of contraception. Both vas deferens are cut and closed to prevent spermatozoa entering the semen.
Prevalence of Vasectomy
Vasectomy use worldwide has declined by 61% in the last two decades; in contrast, tubectomy figures are rising (Jacobstein et al., 2023). Of 922 million women using contraception worldwide, 2% relied on vasectomy compared to 24% who used tubal ligation. The higher the socioeconomic standard or the gender equality, the higher the vasectomy prevalence. Countries with high vasectomy prevalence are Australia (14%), New Zealand (10%), USA (11%), UK(10%), and South Korea (17%). The estimated figures for Germany are significantly lower at 4%. In low- and middle-income countries, the vasectomy prevalence is particularly low (0,6%); in sub-Saharan Africa, the figure is near 0%.
Contraindications of Vasectomy
Coagulation disorders and increased risk for surgery. Vasectomy is not recommended as a short-term form of contraception and should not be offered to men who wish to have children later in their life.
Surgical Technique of Vasectomy
Preoperative Preparations:
- Supine position of the patient
- Lokal anesthesia is the rule; general anesthesia is an option for patients with phobia or contraindications to local anesthetics.
- Perioperative antibiotic prophylaxis if risk factors for surgical site infections are present.
Technique of Local Anesthesia for Vasectomy:
Palpate both vas deferens alternately in the midline of the scrotum below the penis. Infiltrate the scrotal raphe in the area of the planned incision. Infiltrate both vas deferens in the direction of the external inguinal rings with local anesthetic, e.g., lidocaine 1% or ropivacaine 0.5% 5 ml per side. The exposure time should be at least 10 min. Have another syringe with 5–10 ml of local anesthetic ready during the procedure.
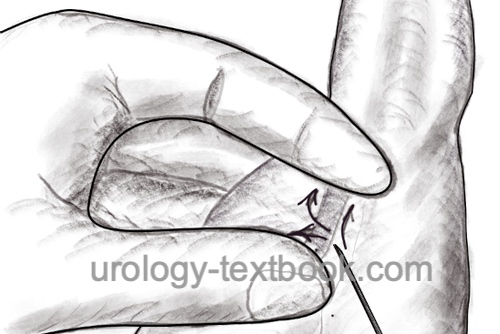 |
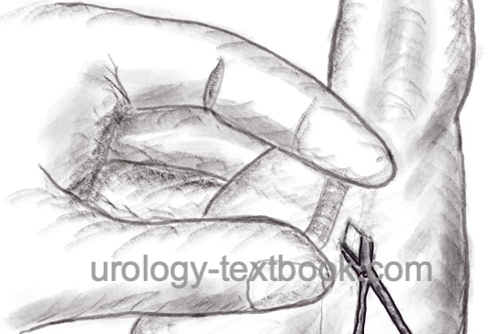
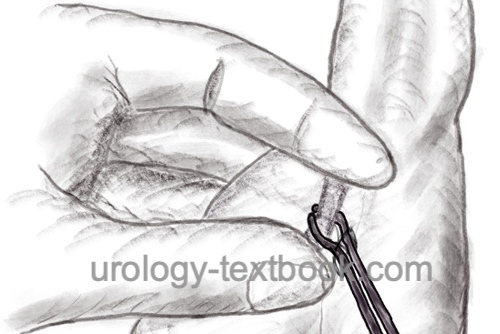
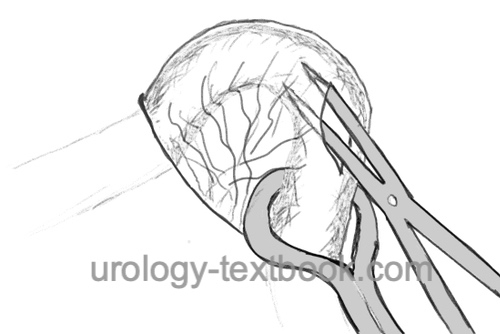
No-Scalpel Vasectomy Procedure:
Grasp the left spermatic cord with the left hand and isolate the vas deferens from the surrounding tissues and vessels between the thumb, index finger, and middle finger in the area of the infiltrated scrotal raphe. Use a special sharp hemostat to puncture and dilate the scrotal skin to about 7 mm. Grasp the vas deferens with a small ring clamp and bring it to the incision. If this step is painful, infiltrate the vas with additional local anesthetic. Spread the layers of tissue over the vas deferens and deliver the vas deferens into the wound. Dissection continues until 3 cm of vas deferens are freed from vessels and nerves. Resect the free segment between the clamps; coagulate and close the ends with sutures. The proximal end is first returned to the scrotum, and the vasal sheath is closed with a suture. Reposition the distal end into the scrotum. Repeat the procedure on the right side similarly through the same wound opening. A skin suture is unnecessary after a no-scalpel vasectomy. A simple dressing for a few days is sufficient.
 |
 |
 |
 |
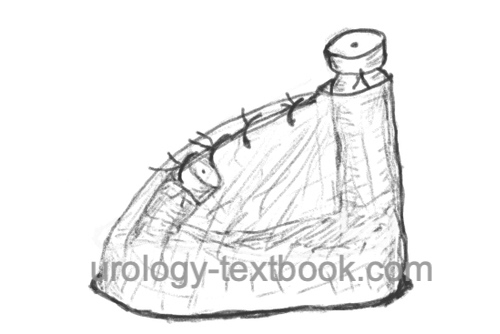 |
Open-ended Vasectomy:
The distal (scrotal) end of the ductus deferens is not coagulated or ligated. Both ends are separated by a fascial interposition described above. Open-ended vasectomy aims at avoiding epididymal back pressure effects and thus reducing post-vasectomy pain. Long-term studies concerning the pearl index are not available.
Follow-up after Vasectomy
Wound examination. Two separate semen analyses should confirm sterility before other methods of contraception are stopped.
Complications (Adverse Effects) after Vasectomy
- Bleeding and hematoma, serious bleeding complications are rare with no-scalpel vasectomy.
- Wound infection (1-2%).
- Persistent or recurrent fertility due to recanalization or double vas deferens (Peacock et al., 2024):
- Early failure rate of 0.9%, post-operative sperm tests are important
- Late failure rate around 0,04%.
- The Pearl index is about 0.1–0.15 after vasectomy, which means 1–2 pregnancies per 1000 women per year.
- Post-Vasectomy Pain Syndrome: is a chronic pain syndrome which develops immediately or several years after vasectomy. The risk is reported to be 0.2% (Peacock et al., 2024) to 1–2% (AUA guidelines), depending on the definition. Several causes have been proposed: nerve injury, sperm granuloma, congestion of the epididymis and chronic inflammation. Treatment options are analgesics, excision of sperm granuloma, denervation of the spermatic cord or vasovasostomy (vasectomy reversal). Long-term studies for treatment success are not available.
| Spermatocelectomy | Index | Testis diseases |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
AUA Guideline: I. D. Sharlip, A. M. Belker, and S. Honig, “Vasectomy.” Accessed: Feb. 15, 2025. [Online]. Available: https://www.auanet.org/guidelines-and-quality/guidelines/vasectomy-guideline
Cook, L. A. u. a. Scalpel versus no-scalpel incision for vasectomy. In: Cochrane Database Syst Rev (2007), S. CD004112.
Jacobstein R, Radloff S, Khan F, Mimno K, Pal M, Snell J, Stafford R, Touré C, Tripathi V. Down But Not Out: Vasectomy Is Faring Poorly Almost Everywhere-We Can Do Better To Make It A True Method Option. Glob Health Sci Pract. 2023 Feb 28;11(1):e2200369. doi: 10.9745/GHSP-D-22-00369.
Peacock J, James G, Atkinson M, Henderson J. Complications of vasectomy: results from a prospective audit of 105 393 procedures. BJU Int. 2024 Nov;134(5):789-795. doi: 10.1111/bju.16463.
 Deutsche Version: Vasektomie
Deutsche Version: Vasektomie
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.