You are here: Urology Textbook > Anatomy > Kidney > Renin-Angiotensin-Aldosterone System
Physiology of the kidney (6/7): Renin-Angiotensin-Aldosterone System
- Anatomy of the kidney (1/7): Gross anatomy
- Anatomy of the kidney (2/7): Histology of the glomerulus and nephron
- Anatomy of the kidney (3/7): Histology of renal tubules
- Anatomy of the kidney (4/7): Physiology of the glomerular filtration rate
- Anatomy of the kidney (5/7): Physiology of the tubular reabsorption
- Anatomy of the kidney (6/7): Physiology of the renin-angiotensin-aldosterone system
- Anatomy of the kidney (7/7): Physiology of erythropoetin, endothelins and vitamin D
Review literature: (Benninghoff, 1993) (Carey and Siragy, 2003) (Schmidt und Thews, 1995).
Function of the Renin-Angiotensin-Aldosterone System (RAAS)
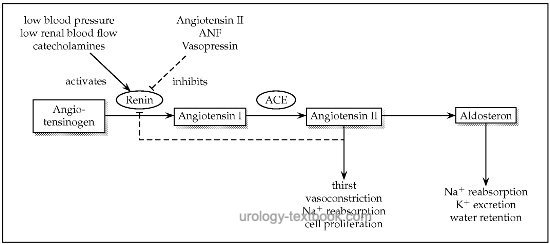
The RAAS plays a central role in blood pressure regulation and consists of a cascade of functional proteins (renin, angiotensinogen, angiotensin I and II) [fig. cascade of the renin-angiotensin-aldosterone system]. The physiological importance of the RAAS is the compensation of hypovolemia, hyponatremia and hypotension. In people with normal blood pressure and a balanced salt homeostasis, the RAAS is not activated. The RAAS receives pathophysiological significance in incorrect activation, e.g., in renal artery stenosis, heart failure or advanced liver disease.
Activation of the Renin-Angiotensin-Aldosterone System (RAAS)
The cascade renin-angiotensin-aldosterone system begins with the cleavage of angiotensinogen to angiotensin I (Ang.I), mediated by renin. This is the rate-determining step. Next, angiotensin-converting enzyme (ACE) cleaves angiotensin I and produces angiotensin II (Ang.II), an extremely potent vasoconstrictor. In addition, Angiotensin II stimulates the release of aldosterone from the adrenal cortex.
 |
Renin
Renin is an aspartyl protease, which specifically cleaves angiotensinogen into angiotensin I (Ang.I). It is the rate-determining step of the RAAS. Renin is produced in the juxtaglomerular cells of the afferent arteriole in the kidney, but is also detected in other organs with a local RAAS.
Control of renin release:
The release of renin requires the uses the adenylate cyclase and formation of cAMP as second messenger system. The following stimuli lead to a renin release with activation of the renin-angiotensin-aldosterone system:
- Macula densa: reduced sodium and chloride concentration in the distal tubule
- Baroreceptors of the afferent arterioles: decreased blood pressure
- Neural mechanisms: the juxtaglomerular cells are innervated by abundant beta-adrenergic sympathetic nerve fibers. Their activation leads to renin secretion.
- Hormonal mechanisms: histamine, dopamine, epinephrine, prostaglandin I2 (prostacyclin) and E2 stimulate renin release. Inhibitory effects have angiotensin II, ANF, endothelin and vasopressin.
Angiotensinogen
The function of angiotensinogen is a serine protease inhibitor. Renin cleaves angiotensinogen into angiotensin I. Angiotensinogen is produced in the liver, but it is also formed in the CNS, kidney, adrenal gland, leukocytes and heart. Angiotensin II, estrogen and glucocorticoids stimulate the synthesis of angiotensinogen, whereas renin is inhibitory.
Angiotensin converting enzyme (ACE)
Angiotensin converting enzyme (ACE) is a zinc-containing glycoprotein with dipeptidyl-carboxy peptidase activity. ACE cleaves two amino acids from angiotensin I, turning it into angiotensin II. Other proteases can also non-specifically activate angiotensin II. Furthermore, ACE inactivates the bradykinin-kallikrein-kinin system. ACE is produced by many endothelial and epithelial cells, the pulmonary activity is very high. For the RAAS, the activity of ACE is not the rate-determining step.
Angiotensin II (Ang.II)
Angiotensin II (Ang.II) is an octapeptide, which is produced by proteolytic cleavage (ACE) of two amino acids from angiotensin I. The following functions are known:
Angiotensin II regulates the glomerular filtration rate:
With a reduced renal perfusion, Ang.II leads to a constriction of the vasa efferentes and thus to an increased filtration pressure. ACE inhibitors can lead to acute renal failure, when given in renal artery stenosis, because the renal perfusion is completely dependent on the RAAS.
Angiotensin II increases the tubular sodium reabsorption and urine concentration:
Ang.II reduces the medullary blood flow; this increases the osmolarity of the renal medulla, the tubular sodium reabsorption and the urine concentration.
Angiotensin II is a potent vasoconstrictor:
Ang.II directly stimulates the smooth muscle contraction in resistance vessels and raises the blood pressure.
Angiotensin II stimulates aldosterone release:
Ang.II acts on the adrenal cortex, causing it to increase aldosterone production and release.
Angiotensin II has effects on the central nerve system:
Ang. II stimulates the blood pressure, increases thirst and salt appetite.
Molecular mode of action of angiotensin II:
The effects of angiotensin II are mediated by angiotensin receptors (AT1 and AT2). The vascular effects of Ang.II are mediated by AT1 receptors. The signal transduction of AT1 receptors starts with G-protein receptors, this leads to an intracellular activation of phospholipase C, DAG, IP3 and protein kinase C. Antagonist to AT1 receptors are the sartans, e.g., losartan, which are used for antihypertensive treatment.
Aldosterone
Aldosterone is a steroid hormone from the adrenal cortex, which influences on the water- and salt balance (mineralocorticoid).
Molecular mode of action of aldosterone:
Aldosterone is lipophil, enters easily the target cell and binds to the nuclear steroid receptor proteins. The activated steroid receptors bind to specific DNA sequences (hormone response elements, HRE) and lead to an increased gene expression.
Aldosterone promotes sodium and water retention, raises the blood pressure and lowers the potassium concentration. The effects of aldosterone take place in several organs:
- Kidneys: increased expression of sodium-potassium pumps, increased luminal permability for Na+ .
- Sweat glands: stimulates Na+ and water reabsorption in exchange for K+
- Gastrointestinal tract: stimulates Na+ and water reabsorption in exchange for K+
| Kidney, reabsorption | Index | Erythropoetin |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Benninghoff 1993 BENNINGHOFF, A.: Makroskopische Anatomie, Embryologie und Histologie des Menschen.15. Auflage.
München; Wien; Baltimore : Urban und Schwarzenberg, 1993
R. M. Carey and H. Siragy.
Newly recognized components of the renin-angiotensin system:
potential roles in cardiovascular and renal regulation.
Endocr Rev, 24 (3): 261–271, Jun 2003.
Schmidt, R. F. & Thews, G. T. (ed.)
Physiologie des Menschen
26. Auflage
Berlin; Heidelberg; New York: Springer, 1995
 Deutsche Version: Physiologie der Nieren: Renin-Angiotensin-Aldosteron System (RAAS).
Deutsche Version: Physiologie der Nieren: Renin-Angiotensin-Aldosteron System (RAAS).
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.