You are here: Urology Textbook > Testes > Varicocele
Varicocele: Causes, Symptoms, and Diagnosis
- Varicocele: Classification, pathophysiology, signs and symptoms
- Varicocele: Treatment (Surgery)
Varicocele: Definition and Classification
A varicocele is defined as ectatic and tortuous veins of the pampiniform plexus of the spermatic cord. Varicoceles are found in 15% of male adolescents and may cause pain, damage to the testes, and infertility. Guidelines: EAU Guideline Paediatric Urology, EAU Guideline Sexual and Reproductive Health AUA Guideline: Infertility in Men.
Classification of Varicoceles
- Subclinical: there is no evidence of a varicocele with inspection or palpation, but reflux is visible with Doppler ultrasound imaging.
- Grade I: not visible, palpable only with a Valsalva maneuver.
- Grade II: not visible, palpable without a Valsalva maneuver.
- Grade III: visible through the scrotum without a Valsalva maneuver
Epidemiology
Varicocele is common; approximately 4–11% of adult males have a varicocele by clinical examination. Over 90% of primary varicoceles are on the left side; right-sided varicoceles are usually less severe and only detectable by Doppler ultrasound imaging. A high BMI decreases the likelihood of varicocele (Rais et al., 2013). The prevalence is up to 30% when Doppler sonography is used for varicocele diagnosis (ChancWalters et al., 2012). The clinical prevalence of varicocele in men with subfertility is 25% (Marmar et al., 2007).
Etiology of Varicocele
Primary Varicoceles
The nearly perpendicular configuration of the renal vein with the left internal spermatic vein combined with incompetent venous valves leads to a long blood column with high pressure in an upright position. The distal internal spermatic vein and pampiniform plexus become ectatic and decompensate. Collaterals develop in the internal and external iliac veins with disease progression.
Secondary Varicocele
A retroperitoneal mass with compression of the internal spermatic vein causes secondary varicoceles. Another cause of secondary varicocele is the Nutcracker syndrome: compression of the left renal vein between the superior mesenteric artery and the aorta.
Pathophysiology of Testicular Dysfunction
Reflux of (Adrenal) Blood
Reflux of adrenal blood increases norepinephrine in the testicular vein and – by diffusion – in the testicular artery, leading to vasoconstriction in the testes. Venous reflux also causes oxidative stress by additional metabolites.
Increased Testicular Temperature
Venous reflux of warm blood from the body's core increases the testicular temperature.
Elevated Venous Pressure
The increased venous pressure impairs the testicular blood flow.
Dysfunction of the Testis
A disturbed function of the germinal epithelium of the testis is the consequence of the factors mentioned above. Varicocele leads to microscopically visible impairment of Sertoli cell function, decreased inhibin secretion, and increased FSH. The impaired blood supply impairs Leydig cell function, resulting in increased LH and sometimes subnormal testosterone concentrations. Markers of subfertility are pathological parameters in the semen analysis (OAT syndrome) and increased DNA fragmentation of the spermatozoa.
Testicular Pathology due to varicocele
Gross Pathology:
Higher grade varicoceles lead to an atrophy of the testis.
Microscopic Pathology:
- Reduction of spermatogenesis with maturation arrest.
- Signs of Leydig cell dysfunction and reduced cell count.
- Tubular thickening and interstitial fibrosis.
- In exceptional cases, Sertoli cell-only syndrome.
Signs and Symptoms of Varicocele
- Usually asymptomatic, varicoceles are often an incidental finding in routine examinations.
- Palpable mass in the spermatic cord, increasing in upright position or with Valsalva maneuver.
- Scrotal pain, especially after a long upright position.
- Testicular atrophy: Normally, the testes size varies by not more than 20% or 2 ml compared to the other side.
- The primary varicocele is almost invariably on the left side. The right (and left) varicocele may be a symptom of a retroperitoneal tumor.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
Diagnosis and Imaging of Varicocele
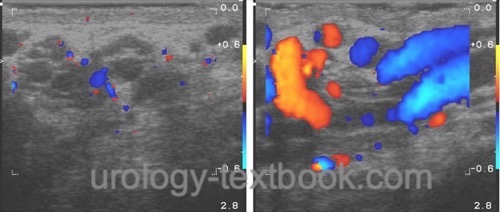
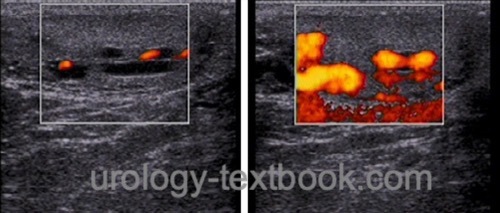
Ultrasound Imaging with Doppler
Signs of varicocele are ectatic veins in the spermatic cord (venous diameter of more than 3.5 mm) and a reduced testicular size (difference >20% or 2 ml). It is essential to exclude testicular or retroperitoneal tumors.
 |
 |
Semen Analysis
Pathological findings in semen analysis (oligozoospermia, asthenozoospermia, teratozoospermia) and DNA fragmentation of spermatozoa are possible. The grading of varicocele correlates with markers of subfertility: for example, up to 55% of men with grade III varicocele have a pathological semen analysis (Damsgaard et al., 2016). Even non-obstructive azoospermia can be caused by a high-grade varicocele.
Laboratory tests:
An elevated FSH and low testosterone are typical for a testicular dysfunction due to a high-grade varicocele.
Scrotal Thermography
Scrotal thermography is an experimental, vague, and unspecific investigation.
| Diseases of the Testes | Index | Varicocele Surgery |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Baazeem, A.; Belzile, E.; Ciampi, A.; Dohle, G.; Jarvi,
K.; Salonia, A.; Weidner, W. & Zini, A.
Varicocele and male factor
infertility treatment: a new meta-analysis and review of the role of
varicocele repair.
Eur Urol, 2011, 60, 796-808.
Bong und Koo 2004 BONG, G. W. ; KOO, H. P.:
The adolescent varicocele: to treat or not to treat.
In: Urol Clin North Am
31 (2004), Nr. 3, S. 509–15, ix
Chanc Walters, R.; Marguet, C. G. & Crain, D. S.
Lower prevalence of varicoceles in obese patients found on routine scrotal
ultrasound.
J. Urol. 2012, 187, 599-601
Evers und Collins 2004 EVERS, J. L. ; COLLINS,
J. A.:
Surgery or embolisation for varicocele in subfertile men.
In: Cochrane Database Syst Rev
(2004), Nr. 3, S. CD000479
Dubin, L. und R. D. Amelar (1970). Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. In: Fertil Steril 21, S. 606–609.
Marmar, J. L.; Agarwal, A.; Prabakaran, S.; Agarwal,
R.; Short, R. A.; Benoff, S. & Thomas, A. J.
Reassessing the value
of varicocelectomy as a treatment for male subfertility with a new
meta-analysis.
Fertil Steril 2007, 88, 639-648
Miller u.a. 2002 MILLER, J ; PFEIFFER, D ;
SCHUMACHER, S ; TAUBER, R ; MüLLER, S. C. ;
WEIDNER, W.:
Die Varicocele testis im Kindes- und Jugendalter.
In: Urologe
41 (2002), S. 68–77
Rais, A.; Zarka, S.; Derazne, E.; Tzur, D.;
Calderon-Margalit, R.; Davidovitch, N.; Afek, A.; Carel, R. & Levine, H.
Varicocoele
among 1 300 000 Israeli adolescent males: time trends and association with
body mass index.
Andrology 2013, 1, 663-669
C. Radmayr, G. Bogaert, H. S. Dogan, and S. Tekgül, “EAU Guidelines: Paediatric Urology.” [Online]. Available: https://uroweb.org/guidelines/paediatric-urology/
Rubenstein u.a. 2004 RUBENSTEIN, R. A. ;
DOGRA, V. S. ; SEFTEL, A. D. ; RESNICK, M. I.:
Benign intrascrotal lesions.
In: J Urol
171 (2004), Nr. 5, S. 1765–72
A. Salonia, S. Minhas, and C. Bettocchi, “EAU Guidelines: Sexual and Reproductive Health.” [Online]. Available: https://uroweb.org/guidelines/sexual-and-reproductive-health/
P. Schlegel, M. Sigman, B. Collura, C. De Jonge, M. Eisenberg, and et al., “Diagnosis and Treatment of Infertility in Men: AUA/ ASRM Guideline.” [Online]. Available: https://www.auanet.org/guidelines-and-quality/guidelines/male-infertility
 Deutsche Version: Varikozele: Ursachen und Folgen
Deutsche Version: Varikozele: Ursachen und Folgen
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.