You are here: Urology Textbook > Kidneys > Nephrolithiasis
Symptoms and Diagnosis of Nephrolithiasis and Renal Colic
- Nephrolithiasis: Etiology and Epidemiology
- Diagnosis of Nephrolithiasis and Renal Colic
- Treatment of Kidney and Ureteral Stones
Signs and Symptoms
Renal colic:
A renal colic is a sudden flank pain, typically changing in intensity, with variable pain radiation depending on the stone location.
- Stone localization in the renal pelvis: colicky (due to stretching of the renal pelvis) or constant (due to stretching of the kidney capsule in the event of obstruction) flank pain.
- Stone localization in the proximal ureter: colicky or constant flank pain with radiation in the lower abdomen.
- Stone localization in the distal ureter: colicky or constant pain in the flank, with radiation in the lower abdomen, scrotum, or large labia with hyperesthesia. Pollakiuria may be present due to irritation of the intramural stone.
Complications of nephrolithiasis:
The impaired urine flow causes upper urinary tract obstruction; there is a risk of infected hydronephrosis with urosepsis. Sudden obstruction can lead to a forniceal rupture with urinoma. Infected obstruction of a renal calyx can lead to a renal abscess. Continuous upper urinary tract obstruction leads to loss of kidney function and, depending on the contralateral kidney function, to kidney failure.
Diagnosis
Diagnostic Evaluation in Renal Colic
Urine sediment:
Typical findings are microhematuria, macrohematuria, and crystalluria.
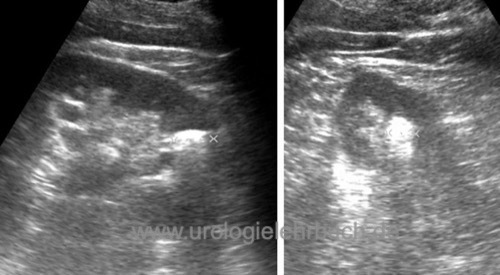
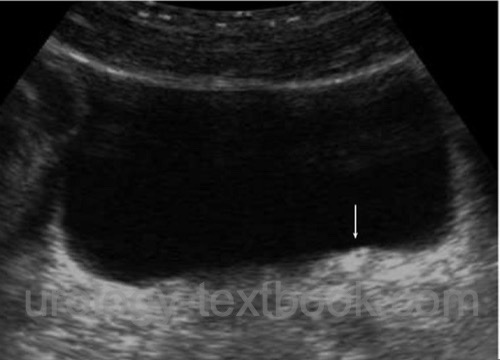
Ultrasound imaging:
Urinary calculi produce an echogenic reflex with dorsal acoustic shadow [fig. ultrasound imaging of calyceal stone and US of renal pelvic stone]. Sonography is efficient in diagnosing stones in the kidney and proximal ureter. With sufficient bladder filling, prevesical urinary stones can be detected [fig. US of prevesical ureteral stone]. Upper urinary tract obstruction is an indirect sign of ureterolithiasis.
 |
 |
 |
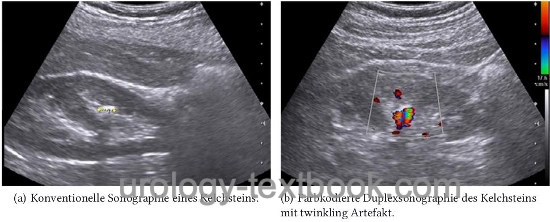
Duplex sonography:
Color-coded duplex sonography can visualize the urine jet into the bladder from the distal ureter. A missing urine jet is an indirect sign of an occluding ureteral stone. The one-sided increase in the resistance index (RI) is also an indirect indicator of acute obstruction. Color-coded duplex sonography also helps identify urinary calculi: the twinkling artifact leads to a rapidly changing color Doppler signal behind the echogenic reflex [fig. twinkling artifact in the kidney and twinkling artifact due to prevesical stone].
 |
 |
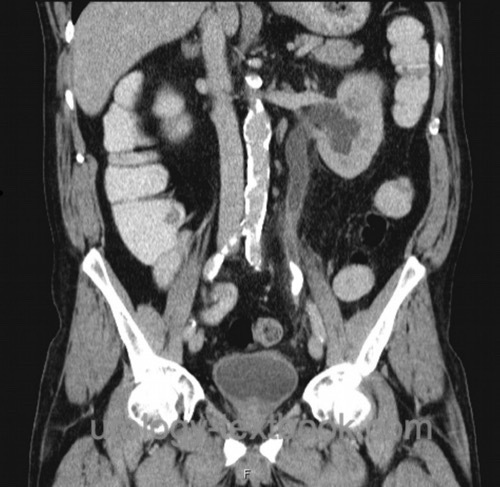
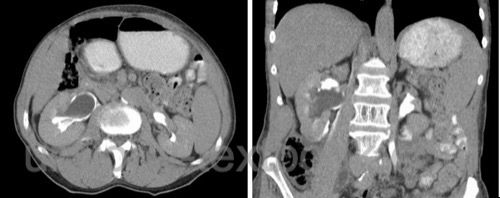
Non-contrast computed tomography (NCCT):
NCCT leads to a quick and reliable diagnosis of urinary calculi, even with low-dose protocols which require only about 2–4 mSv. CT examination has many advantages compared to KUB and IV urography in the diagnosis of renal colic [fig. NCCT of a ureteral stone and hydronephrosis]:
- Can be done during pain episodes
- Avoidance of contrast medium
- Reliable detection of nephrolithiasis and urinary obstruction
- Important differential diagnoses like cholelithiasis, ulcer perforation, ileus, diverticulitis are detected.
Disadvantageous is the missing detailed calyceal and pelvic anatomy imaging to plan the appropriate treatment.
 |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
 |
Intravenous urography:
Intravenous urography is the second choice option if cross-sectional imaging (see NCCT) is unavailable [fig. distal ureteral stone in IVP and proximal ureteral stone in IVP]. Urography cannot be done during renal colic since the increased diuresis by the contrast medium may cause more pain, forniceal rupture, and urinoma [fig. forniceal rupture in IVP and forniceal rupture in CT]. The advantage of urography is imaging the anatomy of the pyelocalyceal system, which is helpful for treatment decisions [fig. staghorn stone].
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
 |
 |
 |
Signs of urolithiasis:
Most kidney stones can be recognized in the KUB as radiopaque shadows in projection onto the urinary tract (except uric acid or xanthine stones). In case of urinary obstruction, contrast medium excretion is delayed, the pyelocalyceal system is dilated, and delayed films (1–2 h after injection) reveal the site of ureteric obstruction. Radiolucent stones present as a filling defect. Rarely, fornix rupture with extravasation develops.
Nephrocalcinosis:
Nephrocalcinosis is a radiological descriptive diagnosis: bilateral deposition of calcium crystals in the renal parenchyma and tubule system, often associated with nephrolithiasis [fig. nephrocalcinosis]. In plain films, multiple calcifications are projected onto the kidneys; radiation-like calcifications correspond to the calcifications in the collecting tubes. The causes of nephrocalcinosis are hypercalciuria (including renal tubular acidosis, hyperparathyroidism, vitamin D intoxication, milk-alkali syndrome, sarcoidosis, tubulopathies, medullary sponge kidney and other genetic causes of hypercalciuria).
 |
Retrograde pyelography:
Retrograde pyelography is indicated for doubtful findings in sonography and urography or before endoscopic therapy.
MRI urography:
MRI urography is indicated for children or pregnant women to avoid radiation exposure or for suspected indinavir stones.
Metabolic Evaluation of Nephrolithiasis
Basic workup:
A basic workup is done for every patient presenting with nephrolithiasis.
History:
Important are former stone episodes, nutrition, medication, and family history.
Urine tests:
Urine sediment and culture, urine pH.
Serum blood tests:
Creatinine, uric acid, sodium, potassium, and calcium.
Extended metabolic workup:
An extended metabolic workup is indicated in patients with a high risk of recurrence (see table risk factors for stone recurrence) or if pathological findings in the basic workup are found. Extended metabolic workup should ideally be done during stone-free intervals.
| High-risk group for recurrent nephrolithiasis | |
| History | More than 3 recurrences in 3 years, children and adolescents, family history with stone formation. |
| Imaging | Single kidney, residual stone fragments after therapy, nephrocalcinosis, bilateral large stone burden. |
| Stone types | Infection stones, brushite stones, uric acid stones, xanthine stones. |
| Genes | Cystinuria (types A, B and C), primary hyperoxaluria, renal tubular acidosis type I, APRT (adenine phosphoribosyl transferase) deficiency, xanthine oxidase deficiency, cystic fibrosis, ADPKD. |
| Other diseases | Hyperparathyroidism, sarcoidosis, gastrointestinal diseases such as Crohn disease, malabsorption, short bowel syndrome or colitis. |
24-hour urine collection:
The following parameters (depending on the stone type) are determined: volume, specific weight, pH, creatinine, calcium, uric acid, oxalate, citrate, sodium, magnesium, phosphate, ammonium, and cystine.
In the case of hypercalciuria, another 24- hour urine collection may be performed after a week of low-sodium and low-calcium diet. If calcium excretion drops below 250 mg/24 h, type II (diet-dependent) absorptive hypercalciuria is present. However, the discrimination between different forms of absorptive hypercalciuria is of little clinical value.
Urine pH profile:
Urine pH is determined for each micturition for one day. Constant pH values above 7 speak for a bacterial infection with the formation of infection stones. Constant pH values above 5.8 are typical for renal tubular acidosis. Constant pH values below 5.8 is a risk factor for calcified and uric acid stones (see above).
Serum blood tests:
Creatinine, urea, uric acid, calcium, phosphate, vitamin D3, and parathyroid hormone.
| Nephrolithiasis | Index | Kidney stone treatment |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Coe u.a. 2005 COE, F. L. ; EVAN, A. ;
WORCESTER, E.:
Kidney stone disease.
In: J Clin Invest
115 (2005), Nr. 10, S. 2598–608
EAU guidelines: Urolithiasis
Moe 2006 MOE, O. W.:
Kidney stones: pathophysiology and medical management.
In: Lancet
367 (2006), Nr. 9507, S. 333–44
 Deutsche Version: Diagnose der Nephrolithiasis und Nierenkolik
Deutsche Version: Diagnose der Nephrolithiasis und Nierenkolik
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.