You are here: Urology Textbook > Penis > Sexually transmitted diseases & Non-gonococcal urethritis
Non-Gonococcal Urethritis (NGU)
Definition
Non-gonococcal urethritis (NGU) is a mucoid (watery, clear discharge) or mucopurulent (whitish, opaque discharge) urethritis that is not caused by Neisseria gonorrhoeae (S3-Leitlinie Urethritis).
Epidemiology of Non-gonococcal Urethritis
The incidence of urethritis in industrialized countries ranges from 200 to 600 cases per 100,000. NGU is now significantly more common than gonorrhea. Risk populations are young sexually active people (2–3% prevalence for urethritis pathogens), especially men who have sex with men (up to 8% prevalence for urethritis pathogens), the majority of whom are asymptomatic.
Causes (Pathogens) of Non-Gonococcal Urethritis
Chlamydia trachomatis:
Chlamydia trachomatis is a gram-negative obligate intracellular bacteria and the most frequent pathogen of NGU. Urethritis is caused by serotypes D–K.
Morphology:
The extracellular forms of Chlamydia are elementary bodies (diameter 0.3 μm); the intracellular multiplication creates intracellular inclusion bodies.
Mycoplasma:
Mycoplasmas are bacteria that lack a cell wall surrounding their cell membrane, are facultative anaerobes, and grow as extracellular parasites on epithelial cells. The detection of Mycoplasma genitalium (17% of NGU) is considered a clear indication of pathology. Other mycoplasmas, such as Mycoplasma hominis, Ureaplasma urealyticum, or parvum, can also be detected in patients without symptoms.
Morphology:
Mycoplasma are spherical to filamentous cells without cell walls; for microscopy, use Giemsa staining. Size between 0.1–0.6 μm.
Bacteria:
Enterococci, E. coli, Haemophilus, Streptococci, Staphylococcus aureus, and Gardnerella vaginalis.
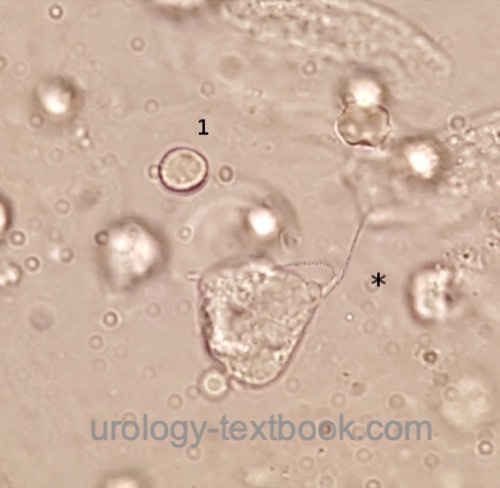
Trichomonas vaginalis:
Trichomonas vaginalis is an parasitic flagellated protozoan and a rare cause of urethritis (<1%). It is very easily detectable in vaginal secretions, and occasionally seen in urine sediment, see fig. Trichomonas vaginalis.
 |
Further causes:
Unknown etiology in 20–30%. Seldom viral urethritis (adenovirus or HSV), mechanical causes (iatrogen, or (self) manipulation).
Signs and Symptoms
Urethritis:
The incubation period is 1–5 weeks. Men complain of glassy or mucopurulent (whitish, opaque discharge) discharge from the urethra, dysuria, burning in the urethra, and balanitis. Women complain of vaginal discharge, dysuria, and abdominal pain (which is a sign of progression to pelvic inflammatory disease). The extent of the symptoms is very variable, and many are asymptomatic.
Complications:
Ascending infections may lead to complications: epididymitis in men and pelvic inflammatory disease (PID) in women. Complications may cause infertility in men and women, which is best documented for PID. The risk for tubal occlusion is around 10\% after the first PID, increasing with the number of episodes. After PID, there is also an increased risk for ectopic pregnancies. Neonates may be infected by their mother (chlamydial conjunctivitis or pneumonia).
Reiter syndrome:
Reiter syndrome is a HLA-B-27-associated autoimmune disease with arthritis, conjunctivitis, balanitis, fever and rashes with cornification at the palms and soles (fig. keratoderma blennorrhagicum). The symptoms develop after a urethritis or gastroenteritis. Due to a mixed infection, the Reiter syndrome is also possible due to gonorrhea.
| Do you want to see the illustration? Please support this website with a Steady membership. In return, you will get access to all images and eliminate the advertisements. Please note: some medical illustrations in urology can be disturbing, shocking, or disgusting for non-specialists. Click here for more information. |
 |
Fitz-Hugh-Curtis syndrome:
Fitz-Hugh-Curtis syndrome is an ascending pelvic inflammatory disease with peritoneal infection. Typical is right-sided abdominal pain due to infection of the hepatic peritoneum (perihepatitis).
Diagnosis
Indications for microbiological testing in men:
Urethral discharge, diagnosis of any other STI, sexual partners with STI, and acute epididymitis in a male under 40 years.
Indications for microbiological testing in women:
Vaginal discharge with risk factors for STI (history, age), diagnosis of any other STI, sexual partners of patients with STI, and acute pelvic inflammatory disease.
Swab tests:
The urethral swab is ideally done after a longer pause in micturition. Further pathogen collection from the anus, pharynx, and cervix depends on history and symptoms. The microbiological diagnosis is possible with different techniques:
NAAT:
With the help of a NAAT (Nucleic Acid Amplification Test), Neisseria gonorrhoeae, Chlamydia trachomatis, and Mycoplasma genitaliumare detected with high sensitivity and specificity.
Microscopic diagnosis:
Microscopic detection of pathogens can distinguish between gonorrheal and non-gonorrheal urethritis more reliably than clinical symptoms, enabling correct empirical antibiotic therapy. It is rarely performed due to the effort involved and the availability of simpler alternatives (NAAT). Two microscope slides for Gram stain (gonococcus) and Giemsa stain (Chlamydia) are prepared if a microscopic pathogen detection is sought.
Test of the sexual partner:
To avoid a ping-pong infection, a detailed history and examination of any sexual partner is necessary.
Urin analysis:
After the urethral swab, urine for culture is collected if a urinary tract infection seems possible.
Serological tests:
Other STDs like syphilis, hepatitis, and HIV should be tested.
Further tests:
In cases of recurrence or chronic urethritis, repeat NAAT (nucleic acid amplification test) for gonorrhea, the pathogens mentioned above, T. vaginalis, and ureaplasma. Perform a swab test and culture for both Gram-negative and Gram-positive bacteria, as well as fungi. Exclude urological, neurological, and orthopedic differential diagnoses.
Treatment of Non-gonococcal Urethritis
When choosing empirical antibiotic therapy, a clinical classification should be made between gonorrheal (characterized by purulent, yellowish discharge) and non-gonorrheal (characterized by watery or whitish discharge) urethritis. In patients without objective symptoms, with minor subjective complaints, who have recently undergone antibiotic therapy for the same complaints, or who have chronic urethritis, the results of the diagnosis should be awaited.
Empirical Standard Treatment:
Standard treatment for non-gonococcal urethritis is doxycyclin 100 mg 1-0-1 p.o. over 7 days.
Empirical Second-Line Therapy:
Azithromycin 1500 mg for five days: 500 mg on day 1 and 250 mg on days 2–5. The German guideline for urethritis recommends a higher off-label dosage of azithromycin over four days: 1000 mg p.o. on the first day and 500 mg p.o. for the next three days. The prolonged therapy is more reliable than the previous standard single-dose therapy with azithromycin 1–2 g p.o. against M. genitalium (S3 Guideline Urethritis).
Treatment of Chlamydia Infection:
First choice is doxycycline 100 mg 1-0-1 p.o. over 7 day. Alternatives are azithromycin 1000 mg p.o. single dosage or 1500 mg over five days (see above), levofloxacin 500 mg p.o. 1-0-0, ofloxacin 300 mg p.o. 1-0-1 or erythromycin 500 mg p.o. 1-1-1-1 for 7 days.
Treatment of Mycoplasma genitalium Infection:
There is a high risk of resistance; ideally, macrolide resistance mutations (MRM) should also be tested. Without MRM: Azithromycin 1500 mg for five days: 500 mg on day 1 and 250 mg on days 2–5. The German guideline for urethritis recommends a higher off-label dosage of azithromycin over four days: 1000 mg p.o. on the first day and 500 mg p.o. for the next three days. Alternatively, if MRM are detected, moxifloxacin 400 mg 1-0-0 is prescribed for 7 days.
Treatment of Trichomoniasis:
Metronidazole 1500 mg to 2000 mg p.o. as a single dose for men. Infections in women are treated over seven days with 500 mg 1-0-1 p.o.
Follow-Up Care and Test of Cure (TOC):
Patients should abstain from sexual activity for two weeks after completing antibiotic therapy and if symptoms persist. Repeat diagnostics after six weeks if symptoms persist or recur. The European guideline does not recommend a test of cure for patients who are symptom-free after a chlamydia infection, in contrast to the German guideline. After infection with Mycoplasma genitalium, a test of cure is uncontroversial.
Prevention:
Treatment of newborn eyes with an antibiotic ointment containing, e.g., tetracycline (Credé prophylaxis), Use of condoms.
Doxycycline post-exposure prophylaxis (Doxy-PEP) against STIs: A single dose of 200 mg doxycycline within three days of unprotected sexual intercourse reduces the risk of chlamydia infection (by 70–80%), syphilis (by 70–80%), and gonorrhea (by 50%) in high-risk patients (Luetkemeyer et al., 2023).
| Gonorrhea | Index | Syphilis |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Center for Disease Control and Prevention: “Sexually Transmitted Infections (STI) Treatment Guidelines,” 2021. [Online]. Available: https://www.cdc.gov/std/treatment-guidelines/STI-Guidelines-2021.pdf
(IUSTI 2025) European Guideline on the management of Chlamydia trachomatis infections: https://iusti.org/wp-content/uploads/2025/03/white-et-al-2025-2025-european-guideline-on-the-management-of-chlamydia-trachomatis-infections.pdf
Luetkemeyer AF, Donnell D, Dombrowski JC, Cohen S, Grabow C, Brown CE, Malinski C, Perkins R, Nasser M, Lopez C, Vittinghoff E, Buchbinder SP, Scott H, Charlebois ED, Havlir DV, Soge OO, Celum C; DoxyPEP Study Team. Postexposure Doxycycline to Prevent Bacterial Sexually Transmitted Infections. N Engl J Med. 2023 Apr 6;388(14):1296-1306. doi: 10.1056/NEJMoa2211934.
RKI Ratgeber zu Chlamydien Infektionen: https://www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_Chlamydiosen_Teil1.html
DDG, DSTIG, DGU, and RKI, “S3-Leitlinie: Management der Urethritis bei männlichen Jugendlichen und Erwachsenen.” [Online]. Available: https://register.awmf.org/assets/guidelines/013-099l_S3_Management-Urethritis-maennliche-Jugendliche-Erwachsene_2025-02.pdf
 Deutsche Version: nichtgonorrhoische Urethritis.
Deutsche Version: nichtgonorrhoische Urethritis.
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.