You are here: Urology Textbook > Adrenal glands > Adrenocortical carcinoma
Diagnosis and Treatment of Adrenocortical Carcinoma
Definition
Adrenocortical carcinoma (ACC) is a very rare, often hormone-producing carcinoma of the adrenal cortex.
Epidemiology
Incidence 1–2/1.000.000, most tumors are detected at an advanced stage with a diameter of 10 cm.
TNM Tumor Stages of Adrenocortical Carcinoma [UICC 2017]
T1:
Primary Tumor.
- T1: Tumor confined to the adrenal and < 5 cm.
- T2: Tumor confined to the adrenal and > 5 cm.
- T3: Tumor infiltrates extraadrenal fat but not neighboring organs.
- T4: Tumor infiltrates neighboring organs.
N:
Regional lymph nodes.
- N0: No regional lymph node metastases
- N1: Metastasis in regional lymph nodes
M:
Distant metastasis
- M0: No distant metastasis
- M1: Distant metastasis
ENSAT Tumor Stages with Prognosis
- Stage I: T1 N0 M0 (five-year survival rate 84%)
- Stage II: T2 N0 M0 (5-YSR 63%)
- Stage III: T3--4 N0--1 M0 oder T1--2 N1 M0 (5-YSR 51%)
- Stage IV: T1--4 N0--1 M1 (5-YSR 15%)
Signs and Symptoms of Adrenocortical Carcinoma
Abdominal or flank pain. Depending on hormone production: Cushing syndrome, virilization, feminization, Conn syndrome. In 20%, there is no (measurable) hormone production.
Diagnosis
Adrenocortical carcinoma is uncommon. Biopsy is contraindicated in tumors of the adrenal glands with a possibility of ACC (risk of tumor seeding). Treatment of adrenal tumors is planned depending on imaging, size, size progression, and hormone production, see the following flow chart.
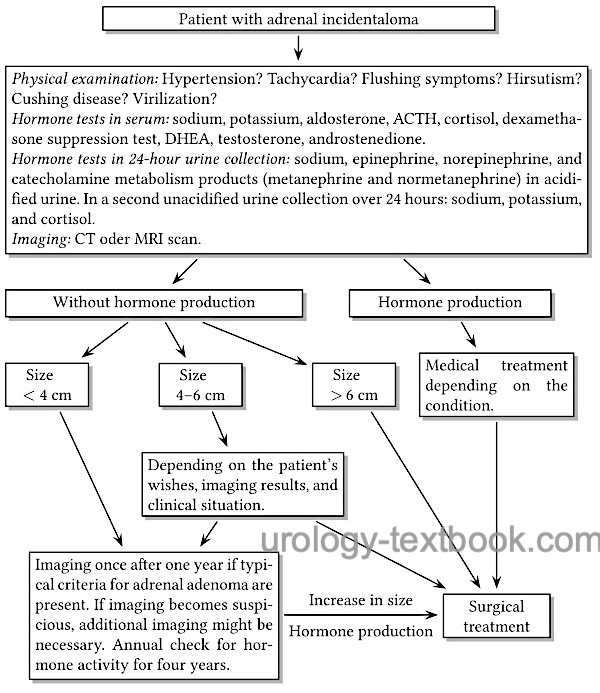 |
Hormone activity:
The hormone activity of the adrenal tumor is determined with blood tests and 24-hour urine collection.
- Serum: sodium, potassium, aldosterone, ACTH, cortisol, dexamethasone suppression test, DHEA, testosterone, androstenedione.
- 24-hour urine collection: sodium, epinephrine, norepinephrine, and catecholamine metabolism products (metanephrine and normetanephrine) in acidified urine. In a second unacidified urine collection over 24 hours: sodium, potassium, cortisol.
- Patients with hypertension: aldosterone/renin quotient in serum.
- Further tests depend on clinical suspicion and the results mentioned above.
Abdominal CT-scan:
An adrenal tumor larger than 5 cm is suspicious for carcinoma [fig. adrenocortical carcinoma]. Furthermore, contrast-enhancing lesions with density values above 10 HU in the native phase (without fat content) should be classified as suspicious (Joudi et al., 2006).
Abdominal MRI:
Larger tumors (over 5 cm) without fat are suspicious for malignancy.
Chest CT:
For staging.
Treatment of Adrenocortical Carcinoma
Adrenalectomy:
Indications for adrenalectomy include any tumors greater than 5–6 cm, hormone-active tumors, and smaller tumors that have progressed in size. If adrenocortical carcinoma is suspected, an open surgical approach with retroperitoneal lymphadenectomy should be chosen, see section adrenalectomy for surgical technique and complications. In advanced tumors, multivisceral en bloc resection may be necessary (splenectomy, resection of kidney, pancreas, bowel, or liver).
Adjuvant therapy:
There is a high risk of recurrence; adjuvant therapy with mitotane and, if necessary, adjuvant radiotherapy of the tumor bed is often recommended. Therapy with mitotane (derivative of a pesticide) leads to inhibition of the adrenal gland with relevant adrenal insufficiency and numerous side effects. Patients with organ-confined tumors, R0 resection, and a low proliferation index of the tumor (Ki-67 below 10%) have the lowest risk of recurrence. Adjuvant therapy is controversial; current studies are ongoing.
Treatment of Metastases:
Less than half of patients respond to chemotherapy; first-line therapy is the EDP/M regimen: etoposide, doxorubicin, cisplatin with mitotane (Fassnacht et al., 2012). Tyrosine kinase inhibitors and checkpoint inhibitors are used in trials.
Prognosis
Prognosis is poor for patients with incomplete resection of adrenocortical carcinoma or metastatic tumor stage; median survival is less than one year. In patients with localized tumor stage and complete resection (T1–2 N0 M0 R0), the five-year survival rate is 84%.
| Pheochromocytoma | Index | Neuroblastoma |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Fassnacht et al. (2018) European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. https://doi.org/10.1530/EJE-18-0608 https://ensat.wildapricot.org/resources/Documents/ACC%20guidelines.pdf
Fassnacht et al., “Combination chemotherapy in advanced adrenocortical carcinoma.,” NEJM, vol. 366, no. 23, pp. 2189–2197, 2012, doi: 10.1056/NEJMoa1200966.
Joudi u.a. 2006 JOUDI, Fadi N. ; KUEHN,
David M. ; WILLIAMS, Richard D.:
Maximizing clinical information obtained by CT.
In: Urol Clin North Am
33 (2006), Aug, Nr. 3, S. 287–300
Ng und Libertino 2003 NG, L. ; LIBERTINO, J. M.:
Adrenocortical carcinoma: diagnosis, evaluation and treatment.
In: J Urol
169 (2003), Nr. 1, S. 5–11
Zini, L.; Porpiglia, F. & Fassnacht, M.
Contemporary
management of adrenocortical carcinoma.
Eur Urol, 2011, 60, 1055-1065.
 Deutsche Version: Diagnose und Therapie des Phäochromozytoms
Deutsche Version: Diagnose und Therapie des Phäochromozytoms
Urology-Textbook.com – Choose the Ad-Free, Professional Resource
This website is designed for physicians and medical professionals. It presents diseases of the genital organs through detailed text and images. Some content may not be suitable for children or sensitive readers. Many illustrations are available exclusively to Steady members. Are you a physician and interested in supporting this project? Join Steady to unlock full access to all images and enjoy an ad-free experience. Try it free for 7 days—no obligation.
New release: The first edition of the Urology Textbook as an e-book—ideal for offline reading and quick reference. With over 1300 pages and hundreds of illustrations, it’s the perfect companion for residents and medical students. After your 7-day trial has ended, you will receive a download link for your exclusive e-book.