You are here: Urology Textbook > Anatomy > Ureter
Anatomy of the Renal Pelvis and Ureter
References: (Benninghoff, 1993).
Gross Anatomy of the Ureter and Renal Pelvis
Renal Pelvis
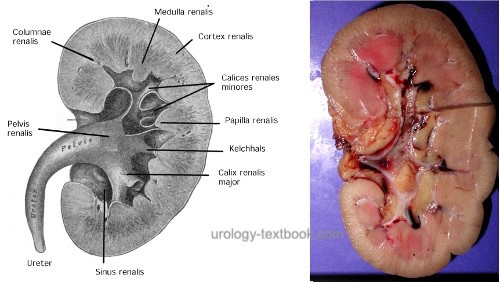
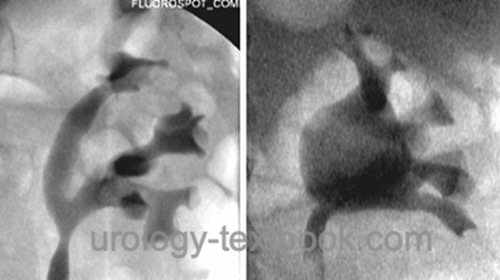
Urine drains from the collecting tubule through the papilla into a minor calyx (calyces minores). Each kidney has 7–9 calyces. Via the calyx necks, several calyces minores drain into two or three calyces majores, which in turn drain into the renal pelvis [fig. anatomy of the renal pelvis and calyces].
Depending on the length and width of the calyces, two different pattern of renal pelvis exist. A dendritic (ramified) pattern refers to long, slim and ramified calyces, the renal pelvis is often divided. The ampullary pattern has short calyces, which drain almost directly into the big and wide renal pelvis. There exist transitions between the two patterns.
 |
The wall of the renal pelvis consists of longitudinal smooth muscle fibers; this enables a milking function of urine from the renal pelvis into the ureter.
Ureter
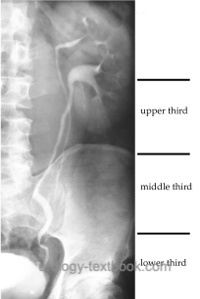
The ureter is a 22–30 cm long muscular tube, which connects renal pelvis and bladder. On radiographs, the ureter is divided into three sections [fig. radiographic anatomy of the ureter]:
- upper third: from renal pelvis to the top edge of the sacrum
- middle third: from the top edge to the lower edge of the sacrum
- distal third: lower edge of the sacrum to the urinary bladder.
 |
Topographic anatomy of the ureter:
The upper third of the ureter lies anterior to the psoas muscle. The transition between the renal pelvis and the ureter causes the upper physiologic narrowing of the ureter. Before reaching the iliac vessels, the ureter lies under the gonadal vessels. The ureter crosses ventrally the iliac vessels; this leads to the middle physiologic narrowing of the ureter. In men, the lower third of the ureter lies dorsally of the vas deferens, the medial umbilical ligament and superior vesical artery. In women, the ureter lies dorsally of the round ligament, uterine artery and above mentioned structures. The transition of the ureters into the bladder causes the lower physiologic narrowing. See section Trigone of the urinary bladder for the anatomy of the ureteral orifice.
Vascular Supply of the Ureter and Renal Pelvis
Arteries of the ureter:
Following arteries give off branches to the pyelocalyceal system and the ureter: renal artery, aorta, gonadal artery, common iliac artery, internal iliac artery, superior vesical artery and in women the uterine artery. In the cranial section of the ureter, the vessels approach the ureter medially. In the caudal section of the ureter, the vessels approach laterally.
A richly branched network of vessels exists in the adventitia of the ureter. This allows the mobilization of the ureter during operations over a long distance without endangering the blood supply.
Veins of the ureter:
Blood from the ureter drains to the renal vein, gonadal vein, internal iliac vein and vesical venous plexus.
Lymphatic vessels of the ureter:
The left upper ureter drains into the paraaortic lymph nodes, the right upper ureter into the paracaval and interaortocaval lymph nodes. The caudal ureter drains into the pelvic lymph nodes (iliac lymph nodes and obturator lymph nodes).
Innervation of the Ureter
The muscle contractions of the ureter are initiated by pacemaker cells in the renal pelvis. The muscle contraction proceeds from cranial to caudal and ensures the urine flow. The autonomic nervous system affects the pacemaker cells in the collecting system.
Parasympathetic innervation of the ureter:
Innervation of the parasympathetic nervous system activates the peristaltic of the ureter. Signals reach the kidney via the vagal nerve and celiac ganglion. Additional supply comes from the sacral parasympathetic system, which (analogous to the embryologic development) reach the kidney via the ureter.
Sympathetic innervation of the ureter:
Sympathetic innervation comes from the sympathetic trunk and regulates the vascular tone.
Pain perception:
Renal and ureteral pain fibers are activated by stretching the collecting system and ureter. Additional pain triggers are a direct injury to the mucosa. The pain stimuli are transmitted together with sympathetic fibers and produce a typical visceral pain. The reflex-like activation of the subcostal nerve, genitofemoral nerve and ilioinguinal nerve produces a pain with radiating to the flanks, groin and genital region with hyperalgesia.
Histology of the Ureter
Mucosa:
The ureter is lined with transitional epithelium (urothelium) of 4–5 cell layers.
Lamina propria mucosae:
Beneath the urothelium there is a elastic Lamina propria with connective tissue and vessels.
Tunica muscularis:
The tunica muscularis of the ureter is composed of smooth muscle. The inner layer consists of longitudinal muscle fibers and the outer layer of circular muscle fibers. The distal third of the ureter has a additional outer layer of longitudinal fibers.
Adventitia:
The ureter is surrounded with connective tissue and a rich vascular plexus.
| Anatomy | Index | Bladder, Anatomy |
Index: 1–9 A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
References
Benninghoff 1993 BENNINGHOFF, A.:
Makroskopische Anatomie, Embryologie und Histologie des
Menschen.
15. Auflage.
München; Wien; Baltimore : Urban und Schwarzenberg, 1993
 Deutsche Version: Anatomie der Harnleiter (Ureter).
Deutsche Version: Anatomie der Harnleiter (Ureter).